Journey through the annals of medical history as we delve into the remarkable odyssey of tuberculosis treatment, a tale that spans centuries and continents. From ancient remedies rooted in folklore to modern cures born of scientific ingenuity, witness the evolution of humanity’s relentless battle against this formidable disease in [History of Tuberculosis Treatment: A Journey from Ancient Remedies to Modern Cures].
Key Takeaways:
- In 1944, the discovery of effective medications, such as streptomycin and para-aminosalicylic acid, led to successful treatment outcomes for many tuberculosis cases.
- The introduction of “triple therapy” in 1952, which combined streptomycin, para-aminosalicylic acid, and isoniazid, provided a more reliable and efficient cure.
- The 1970s marked a significant advancement when it was discovered that isoniazid and rifampin could be used together to shorten the duration of tuberculosis treatment.
- The development of para-aminosalicyclic acid (PAS), an oral agent, further expanded treatment options.
- The introduction of antibiotics, particularly streptomycin, in 1944 represented a pivotal moment in tuberculosis therapy, although its use led to the development of antibiotic resistance.
History of Tuberculosis Treatment:
The annals of Tuberculosis (TB) Treatment bear witness to a relentless pursuit of remedies dating back centuries. From the earliest civilizations to the advent of modern medicine, humankind’s quest to combat this deadly disease has been marked by both triumph and tribulation.
Unveiling the Past: Ancient Remedies and Early Discoveries
In ancient times, TB was shrouded in mystery and often attributed to supernatural causes. Treatment methods varied widely, reflecting the beliefs and practices of different cultures. Traditional healers employed herbal concoctions, bloodletting, and isolation as primary remedies, with varying degrees of success.
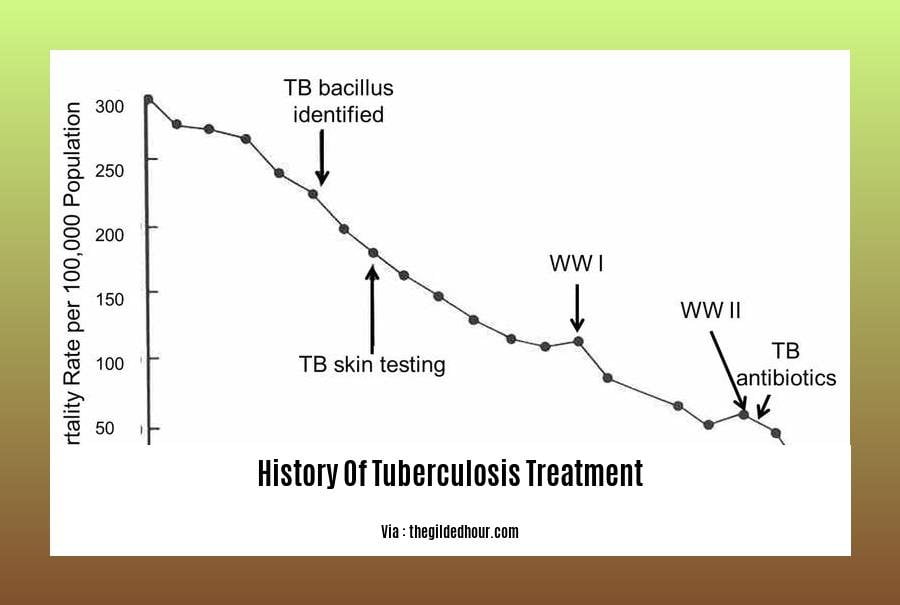
The advent of scientific inquiry ushered in a new era in TB treatment. In the 19th century, the identification of the causative agent, Mycobacterium tuberculosis, marked a pivotal moment. This discovery paved the way for the development of diagnostic techniques, enabling targeted interventions and monitoring treatment progress.
Sanatoriums: A Haven for Healing and Recovery
The early 20th century witnessed the rise of sanatoriums, specialized healthcare facilities dedicated to TB treatment. These institutions provided a controlled environment, emphasizing rest, fresh air, sunlight, and a nutritious diet. Sanatoriums also played a crucial role in isolating infectious individuals, helping to prevent the spread of the disease.
Anti-Tuberculosis Drugs: A Turning Point in TB Management
The discovery of effective anti-tuberculosis drugs in the mid-20th century revolutionized TB treatment. Streptomycin, the first effective drug against TB, was isolated in 1944, followed by para-aminosalicylic acid (PAS) and isoniazid. The introduction of these drugs marked a turning point in the fight against TB, significantly reducing mortality rates and offering hope for a cure.
The Ongoing Battle: Multidrug-Resistant Tuberculosis and New Frontiers
Despite these advancements, the emergence of multidrug-resistant tuberculosis (MDR-TB) posed a significant challenge. MDR-TB strains exhibit resistance to multiple first-line anti-tuberculosis drugs, complicating treatment and necessitating prolonged and intensive regimens.
Current research efforts focus on developing new drugs, improving treatment regimens, and exploring innovative approaches to prevent the spread of tuberculosis. Promising avenues include personalized medicine, gene editing, and the development of new vaccines.
A Continued Journey Towards Eradication
The History of Tuberculosis Treatment reflects humanity’s unwavering commitment to combating this devastating disease. From ancient remedies to modern medical interventions, the journey has been marked by both progress and challenges. As we continue to delve deeper into the complexities of TB, the hope remains that one day, this global health threat will be eradicated.
Find out how Tuberculosis evolved throughout history and its impact on global health.
Learn how History Of Tuberculosis Icd 10 is classified and its significance in the diagnosis and tracking of the disease.
Discover the journey of History Of Tuberculosis In The United States from its early origins to present-day efforts in prevention and treatment.
Explore the breakthroughs and challenges in the development of the History Of Tuberculosis Vaccine, aiming to eradicate this century-old disease.
Delve into the history of History Of Tuberculosis In Africa and understand the unique challenges faced by the continent in combating this disease.
Sanatorium Movement: A Pivotal Era in Tuberculosis Treatment
In the annals of medical history, the Sanatorium Movement stands as a beacon of hope against the ravages of tuberculosis. Emerging during the 19th century when tuberculosis wreaked havoc across the globe, sanatoriums provided a sanctuary for patients to heal, recover, and reclaim their lives. Step into the world of sanatoriums, where fresh air, rest, and medical care converged to combat a deadly disease.
Key Takeaways:
- Sanatoriums emerged in the 1800s as specialized facilities dedicated to tuberculosis treatment, offering isolation, rest, and fresh air therapy.
- The movement gained momentum as tuberculosis became a leading cause of death in Europe and North America, with sanatoriums providing specialized care and a structured routine for patients.
- Sanatoriums combined aspects of hospitals and resorts, emphasizing patient comfort and health outcomes, with regimented routines and isolation forming the core of the treatment approach.
- The Sanatorium Movement not only impacted tuberculosis treatment but also influenced the care of patients with all forms of the disease, contributing to advancements and understanding.
Sanatoriums: A Haven for Healing
Picture a place nestled amidst serene landscapes, where the soft whisper of leaves carried the promise of renewal. Sanatoriums were havens of tranquility, where patients sought respite from the relentless grip of tuberculosis. Surrounded by nature, they found solace in the healing power of fresh air and sunlight.
Sanatoriums operated on the philosophy that rest and relaxation were essential for recovery. Patients were encouraged to spend hours outdoors, basking in the sun’s warm embrace. They participated in leisurely activities like walking, gardening, or simply reclining in the open air. The focus was on promoting physical and mental well-being, fostering a sense of calm and tranquility.
Structured Routine: A Path to Recovery
Life within sanatoriums revolved around a structured routine meticulously designed to promote healing. Patients adhered to regimented schedules that included mealtimes, rest periods, and medical check-ups. This routine provided a sense of order and predictability, helping patients cope with the uncertainties of their condition.
Sanatoriums also emphasized the importance of a nutritious diet. Meals were carefully planned to provide patients with the necessary nutrients to support their recovery. Fresh fruits, vegetables, and wholesome foods were the cornerstones of sanatorium cuisine, bolstering the immune system and aiding in the healing process.
Medical Care: Advancing the Fight Against Tuberculosis
While rest and fresh air were the mainstays of sanatorium treatment, medical care played a crucial role in combating tuberculosis. Physicians closely monitored patients, providing supportive care and administering medications to alleviate symptoms and prevent complications.
As medical knowledge evolved, sanatoriums witnessed the introduction of groundbreaking treatments. The discovery of streptomycin in the 1940s marked a turning point, offering hope for a cure. This was followed by the development of other effective drugs, revolutionizing tuberculosis treatment and significantly reducing mortality rates.
A Legacy of Hope and Healing
The Sanatorium Movement left an indelible mark on the history of tuberculosis treatment. Sanatoriums provided a lifeline to countless patients, offering a chance to reclaim their health and rebuild their lives. They fostered a sense of community and support, where patients found solace and strength amidst shared experiences.
Today, tuberculosis remains a global health concern, but the specter of death and despair that once haunted the disease has been diminished. The lessons learned from the Sanatorium Movement continue to inform modern treatment approaches, underscoring the importance of rest, fresh air, and a supportive environment in promoting healing.
Citation:
- The History of Tuberculosis: The Social Role of Sanatoria for the Treatment of Pulmonary Tuberculosis
- The Sanatorium Movement in America
Anti-Tuberculosis Drugs
Who would have thought a disease that was a death sentence centuries ago would become manageable with the help of modern medicine?
The discovery of anti-tuberculosis drugs has revolutionized the medical world and, more importantly, the lives of millions of people suffering from tuberculosis (TB). From ancient remedies to cutting-edge treatments, the journey of fighting TB has been one of determination and resilience.
Key Takeaways:
- Sanatoriums provided isolation, rest, fresh air, and nutritious food for TB patients.
- The development of anti-tuberculosis drugs was a major breakthrough in TB treatment.
- Multidrug-resistant TB is a major challenge in TB control.
- Ongoing research is focused on developing new drugs and improving treatment regimens for TB.
The Evolution of Tuberculosis Treatment
In the early days, TB was treated with a variety of traditional remedies, including herbal concoctions and bloodletting. However, it was the discovery of anti-tuberculosis drugs in the mid-20th century that marked a turning point in the fight against TB.
Anti-tuberculosis drugs such as streptomycin, isoniazid, and rifampicin have significantly reduced TB mortality rates and improved treatment outcomes. These drugs work by targeting different aspects of the TB bacteria, inhibiting their growth and reproduction.
The Challenge of Multidrug-Resistant TB
Despite the success of anti-tuberculosis drugs, the emergence of multidrug-resistant TB (MDR-TB) has posed a major challenge to TB control. MDR-TB is caused by strains of TB bacteria that are resistant to at least two of the first-line anti-tuberculosis drugs.
The treatment of MDR-TB is complex and requires the use of second-line drugs, which are often more toxic and less effective than first-line drugs. The duration of treatment for MDR-TB is also longer, and success rates are lower.
Looking Ahead
Researchers worldwide continue to work tirelessly to develop new anti-tuberculosis drugs and improve treatment regimens. One promising area of research is the development of shorter treatment regimens that are more patient-friendly and reduce the risk of drug resistance.
The battle against TB is far from over, but the progress made in the development of anti-tuberculosis drugs has given us hope that one day we will be able to eradicate this deadly disease.
Sources:
Multidrug-Resistant Tuberculosis: A Global Health Challenge
Key Takeaways:
- Multidrug-Resistant Tuberculosis (MDR-TB): A strain of tuberculosis that resists at least two of the most effective first-line anti-TB drugs, isoniazid and rifampicin.
- Emergence of MDR-TB: Caused by improper treatment, poor adherence to treatment regimens, and inadequate infection control measures.
- Challenges in Treating MDR-TB: Treatment options are limited and often require longer treatment durations, more expensive drugs, and increased side effects.
- Global Impact: MDR-TB is estimated to account for approximately 3.4% of new TB cases and 20% of previously treated TB cases worldwide.
- Drug Development Efforts: Ongoing research is focused on developing new drugs and treatment regimens to combat MDR-TB, including shorter treatment durations and improved tolerability.
Understanding MDR-TB:
- Drug-resistant tuberculosis (TB) is a growing public health concern.
- MDR-TB is a strain of TB that is resistant to at least two of the most effective first-line anti-TB drugs: isoniazid and rifampicin.
- It is often associated with
_
1. Improper treatment _
_
2. Poor adherence to treatment regimens _
_
3. Inadequate infection control measures _
_
- MDR-TB is a major threat, as it can significantly complicate treatment and make it less effective or require alternative drugs, which can be toxic or expensive.
Challenges in Treating MDR-TB:
- Treating MDR-TB can be challenging due to several factors:
_
1. Limited treatment options _
_
2. Longer treatment durations (up to 2 years or more) _
_
3. Increased risk of side effects from medications due to drug resistance _
_
4. Higher cost of treatment _
_
- The emergence of MDR-TB highlights the need for continued research and development of new drugs and treatment strategies.
Global Impact of MDR-TB:
- MDR-TB is a significant public health concern globally, affecting millions worldwide:
_
1. Approximately 3.4% of new TB cases and 20% of previously treated TB cases worldwide are estimated to be MDR-TB _
_
2. MDR-TB is reported in 117 countries and poses a threat to global TB control efforts _
Developing New Treatments for MDR-TB:
Scientists and researchers worldwide are actively engaged in developing new drugs and treatment strategies to combat MDR-TB.
The focus is on:
_
1. Developing shorter treatment durations, reducing the risk of drug resistance and improving adherence _
_
2. Improving the tolerability of treatment regimens to minimize side effects _
_
3. Investigating new drugs and drug combinations that are effective against MDR-TB strains _
_
- These efforts aim to make MDR-TB treatment more effective, accessible, and affordable.
Conclusion:
MDR-TB is a serious public health concern requiring urgent attention. It poses challenges in treatment and control and has significant implications for global TB efforts. Continued research and development of new drugs and treatment strategies are crucial to combat MDR-TB and ultimately reduce its global impact.
Sources:
World Health Organization: Multidrug-Resistant Tuberculosis (MDR-TB)
Centers for Disease Control and Prevention: Multidrug-Resistant Tuberculosis (MDR-TB)
FAQ
Q1: What were the earliest treatments for tuberculosis?
A1: In ancient times, treatments for tuberculosis were limited and often ineffective. Traditional remedies included herbal concoctions, bloodletting, and changes in diet. Some cultures believed that fresh air and sunlight could help cure the disease, leading to the establishment of sanatoriums in the 19th century.
Q2: When were the first effective medications for tuberculosis discovered?
A2: The discovery of streptomycin in 1944 marked a significant turning point in the treatment of tuberculosis. It was the first antibiotic found to be effective against the disease and led to the development of combination therapies that significantly improved cure rates.
Q3: How has the treatment of tuberculosis evolved over time?
A3: The evolution of tuberculosis treatment has been driven by advances in medical research and the emergence of drug resistance. The introduction of multi-drug therapy in the 1950s improved treatment outcomes, and the development of newer drugs like rifampin and isoniazid further shortened treatment duration. Ongoing research continues to explore new and more effective treatment options.
Q4: What are the challenges in treating tuberculosis today?
A4: One of the major challenges in treating tuberculosis today is the emergence of drug-resistant strains. Multidrug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) are difficult to treat and require longer and more complex treatment regimens. Additionally, the long duration of treatment can lead to poor patient adherence, contributing to the development of drug resistance.
Q5: What are the prospects for future treatments for tuberculosis?
A5: Researchers are actively pursuing the development of new drugs and treatment strategies to combat tuberculosis. One promising area of research is the development of shorter treatment regimens that can reduce the risk of drug resistance and improve patient adherence. Additionally, scientists are exploring host-directed therapies that aim to enhance the immune system’s ability to fight the infection.
- China II Review: Delicious Food & Speedy Service - April 17, 2025
- Understand Virginia’s Flag: History & Debate - April 17, 2025
- Explore Long Island’s Map: Unique Regions & Insights - April 17, 2025