[- A Comprehensive Look at the History of Tuberculosis in the United States -] Tuberculosis, a contagious infectious disease that primarily affects the lungs, has played a pivotal role in shaping public health in the United States. Throughout history, it has left an indelible mark on society, influencing medical advancements, public health policies, and the collective understanding of infectious diseases. This article delves into the intricate tapestry of tuberculosis in the United States, exploring its historical roots, tracing its evolution, and examining the multifaceted societal and medical responses to this formidable disease.
Key Takeaways:
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis (MT), affecting both humans and animals.
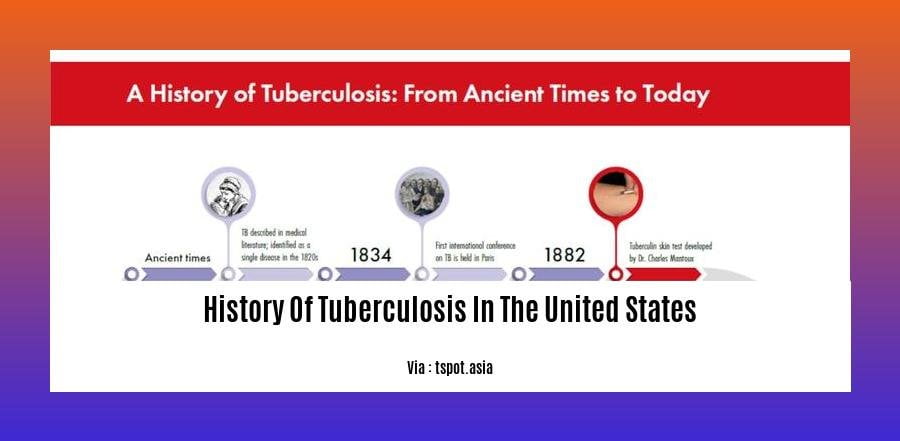
TB has a long history, with evidence of the disease dating back thousands of years.
In the 18th and 19th centuries, TB became epidemic in Europe, causing high mortality rates.
The 20th century saw significant advancements in understanding TB transmission, leading to improved treatments and preventive measures, including the development of a vaccine.
Despite these advancements, TB remains a global health challenge, with millions of new cases and deaths reported annually.
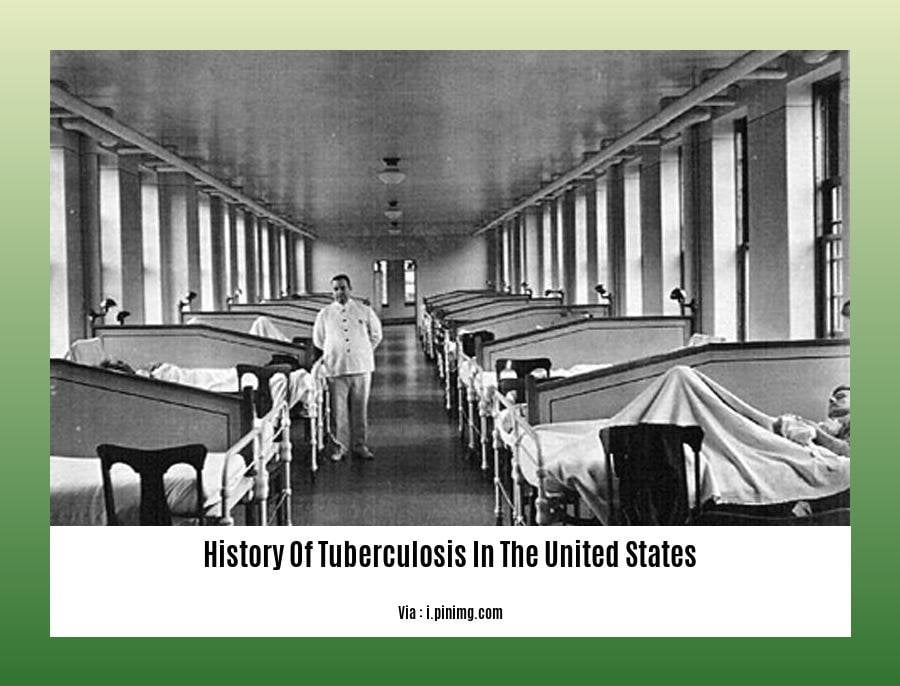
History Of Tuberculosis In The United States
Tuberculosis, an age-old contagious disease, has had a substantial impact on the health and society of the United States. Let’s delve into its intricate history:
Early Presence and Prevalence
From the time European settlers set foot on American soil, Tuberculosis (TB) was already a stealthy presence among the indigenous population. But as the 18th and 19th centuries unfolded, it morphed into a full-blown epidemic, particularly in cramped urban areas. The disease spread like wildfire, claiming countless lives.
The Rise of Sanatoriums and Treatments
Recognizing the devastating toll of TB, the United States responded with a concerted effort. Sanatoriums, specialized facilities dedicated to isolating and treating TB patients, sprang up across the country. These institutions provided much-needed respite and care, fostering a sense of community and support.
Meanwhile, the medical community was racing against time to develop effective treatments. The discovery of antibiotics in the early 20th century proved a game-changer. Drugs like streptomycin and isoniazid became potent weapons in the fight against TB, offering a glimmer of hope to countless patients.
Public Health Measures and Declining Incidence
Public health initiatives also played a pivotal role in curbing the TB epidemic. Widespread screening programs, coupled with aggressive contact tracing and vaccination campaigns, significantly reduced the prevalence of the disease. As living conditions improved and nutrition became more accessible, TB’s hold on the nation began to weaken.
MDR-TB: A New Challenge
Despite these advancements, the battle against TB was far from over. In recent decades, a formidable foe emerged – multi-drug-resistant TB (MDR-TB), a strain that exhibits resistance to multiple first-line antibiotics. This development posed a serious threat, emphasizing the need for continued vigilance and research.
The Road Ahead
While TB remains a persistent concern, remarkable progress has been made in understanding, treating, and preventing the disease. Yet, challenges remain. Ensuring equitable access to healthcare, addressing social determinants of health, and developing new and more effective treatments are just a few of the hurdles that must be overcome.
We must remain steadfast in our commitment to eradicating TB. By harnessing scientific advancements, strengthening public health measures, and fostering collaboration among stakeholders, we can create a future where Tuberculosis (TB) is a relic of the past.
Travel back in time to unravel the intricate history of tuberculosis, a disease that has woven its thread through history.
Delve into the intricacies of History Of Tuberculosis Icd 10 and uncover the codes that illuminate the complexities of this age-old affliction.
Dive into the annals of History Of Tuberculosis Treatment and witness the evolution of strategies to combat this resilient foe.
Explore the pioneering strides made in History Of Tuberculosis Vaccine, a beacon of hope against a persistent adversary.
Embark on a journey through History Of Tuberculosis In Africa, a continent grappling with the enduring grasp of this formidable foe.
Decline of Tuberculosis in the US During the 20th Century: Improved Living, Nutrition, and Antibiotics
In the early 1900s, tuberculosis (TB) was a leading cause of death in the United States. But over the course of the 20th century, TB rates declined dramatically, thanks to several key factors:
Improved Living Conditions: One major factor in the decline of TB was the improvement in living conditions in the United States. As people moved from crowded, unsanitary slums to more spacious, well-ventilated homes, the risk of TB transmission decreased.
Better Nutrition: As the standard of living improved in the United States, people began to have access to a more nutritious diet. This helped to boost their immune systems and made them less susceptible to TB infection.
Discovery of effective Antibiotics: The development of effective antibiotics in the mid-20th century was a major breakthrough in the fight against TB. Drugs like streptomycin and isoniazid revolutionized treatment, making it possible to cure TB in most cases.
As a result of these factors, the TB rate in the United States plummeted from 200 cases per 100,000 people in 1900 to less than 1 case per 100,000 people by the end of the 20th century.
Key Takeaways:
- Improved living conditions: Less crowded housing, better ventilation, and improved sanitation reduced the risk of TB transmission.
- Better nutrition: A more nutritious diet helped boost people’s immune systems and made them less susceptible to TB infection.
- Discovery of effective antibiotics: Drugs like streptomycin and isoniazid revolutionized treatment, making it possible to cure TB in most cases.
Citations:
[1] Centers for Disease Control and Prevention. (2023, March 17). Tuberculosis (TB). Retrieved from https://www.cdc.gov/tb/
[2] National Library of Medicine. (2022, July 20). Tuberculosis (TB). Retrieved from
Emergence of multi-drug resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) in recent years, and the challenges they pose to tuberculosis control.
Tuberculosis (TB) is a curable disease, but it can be fatal if not treated properly. In recent years, there has been an emergence of multi-drug resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB), which pose significant challenges to TB control. These emerging strains of TB are resistant to the most commonly used anti-tuberculosis drugs, making them difficult to treat and requiring prolonged and expensive treatment regimens.
Key Takeaway:
Increased Complexity of Treatment: Treating MDR-TB and XDR-TB requires complex treatment regimens, often involving combinations of several drugs, which can be difficult to manage and can lead to side effects.
Reduced Treatment Success: Due to drug resistance, MDR-TB and XDR-TB are more challenging to treat, resulting in lower cure rates and increased risk of treatment failure.
Transmission Concerns: MDR-TB and XDR-TB can be transmitted through the air, just like regular TB. This poses a public health concern as it can result in the spread of drug-resistant TB strains within communities, making it harder to contain outbreaks.
Limited Treatment Options: There are fewer effective treatment options available for MDR-TB and XDR-TB compared to regular TB, making it even more challenging to find appropriate medications.
High Costs: Treating MDR-TB and XDR-TB is significantly more expensive than regular TB due to the prolonged treatment duration, the need for specialized medications, and the increased healthcare resources required.
Addressing the challenges posed by MDR-TB and XDR-TB requires a multifaceted approach, including:
Strengthening Surveillance and Diagnostic Capacity: Implementing robust surveillance systems to monitor the prevalence and spread of MDR-TB and XDR-TB, and ensuring access to accurate and rapid diagnostic tests.
Developing New Drugs and Treatment Regimens: Investing in research and development to create more effective and affordable drugs that can target MDR-TB and XDR-TB strains.
Improving Patient Care and Support: Providing comprehensive care and support for patients with MDR-TB and XDR-TB, including access to counseling, social support, and adherence to treatment.
Enhancing Infection Control Measures: Implementing strict infection control measures in healthcare settings and communities to prevent the spread of MDR-TB and XDR-TB.
Promoting Collaboration and Partnerships: Fostering collaboration among healthcare providers, public health agencies, researchers, and communities to develop comprehensive strategies for addressing MDR-TB and XDR-TB.
By addressing these challenges and implementing effective interventions, we can work towards controlling the spread of MDR-TB and XDR-TB and ultimately improve the lives of those affected by this deadly disease.
Citations:
Tuberculosis: Multidrug-resistant tuberculosis (MDR-TB)
Role of Public Health Agencies in Tuberculosis Control
Tuberculosis, an infectious disease transmitted through the air, posed a serious public health challenge in the United States. It took the concerted effort of public health agencies and medical professionals to bring the infection under control. Their contributions are evident in the declining TB cases, leading to its near elimination.
Key Takeaways:
- Public health agencies played a pivotal role in identifying and treating TB cases, providing preventive care, and implementing control measures.
- Enhanced surveillance, contact tracing, and isolation protocols helped contain the spread of infection.
- Public awareness campaigns and education programs played a crucial role in preventing the spread of TB and promoting early detection.
- Collaboration among federal, state, and local health agencies ensured a comprehensive and coordinated response to TB control.
- Ongoing research and development of new diagnostic tools, treatments, and vaccines contributed significantly to the decline in TB incidence.
Public health agencies worked tirelessly to contain the spread of TB. They focused on the following three core strategies:
- Identifying and treating individuals with active TB disease:
- Public health agencies conducted extensive screening and testing programs to identify individuals with TB infection or disease.
They provided treatment regimens and ensured adherence to complete the treatment, reducing the risk of transmission and promoting recovery.
Finding and evaluating individuals exposed to TB:
- Contact tracing was employed to identify individuals who came into close contact with an infected individual.
These individuals were evaluated for TB infection and, if necessary, provided preventive treatment to prevent the development of active disease.
Providing preventive treatment to individuals at risk of TB disease:
- Public health agencies identified individuals at high risk of developing TB, such as those with weakened immune systems or those living in close contact with an infected person.
- They provided preventive treatment to these individuals to reduce their risk of developing active TB disease.
Public health agencies also worked to improve living conditions, which played a vital role in reducing the spread of TB. They focused on providing access to adequate housing, clean water, and proper sanitation, as well as addressing overcrowding and improving ventilation in public spaces.
Public health agencies continue to play a critical role in TB control and prevention. They monitor TB trends, evaluate new diagnostic and treatment methods, and conduct research to better understand the disease. By working together, public health agencies, healthcare providers, and communities can work toward the goal of eliminating TB in the United States.
Sources:
[1]
[2]
FAQ
Q1: What is the history of tuberculosis in the United States?
A1: Tuberculosis (TB) has a long history in the United States, with significant declines in incidence rates observed in the 20th century due to improved living conditions, public health measures, and the use of anti-tuberculosis drugs. However, resurgence occurred in the 1990s due to factors like the HIV epidemic and multidrug-resistant TB, leading to renewed efforts in TB control and prevention.
Q2: What are the key periods of decline in tuberculosis incidence rates in the United States?
A2: There were two major periods of decline in TB incidence rates in the United States. The first occurred between 1900 and 1950 due to improvements in living conditions and public health measures, while the second took place between 1950 and 1985 due to the widespread use of anti-tuberculosis drugs.
Q3: What is multidrug-resistant tuberculosis (MDR-TB), and why is it a concern?
A3: Multidrug-resistant tuberculosis (MDR-TB) is a form of TB that is resistant to the standard first-line treatment drugs, isoniazid and rifampicin. It is a serious concern because it is difficult to treat and can lead to poor outcomes for patients.
Q4: How has public health played a role in controlling and preventing tuberculosis in the United States?
A4: Public health measures, such as isolation, contact tracing, and improved living conditions, have been instrumental in controlling and preventing tuberculosis in the United States. Public health agencies at various levels have the responsibility for TB control and prevention, implementing strategies for case identification and treatment, preventive therapy, and infection control.
Q5: What has caused the resurgence of tuberculosis in the 1990s, and how has the United States responded?
A5: The resurgence of tuberculosis in the 1990s was attributed to factors such as the HIV epidemic, the emergence of multidrug-resistant TB, and increased immigration from high-TB-burden countries. In response, the United States implemented comprehensive TB control programs, including enhanced case finding, treatment, and prevention measures, leading to a steady decline in TB incidence rates since 2000.
- China II Review: Delicious Food & Speedy Service - April 17, 2025
- Understand Virginia’s Flag: History & Debate - April 17, 2025
- Explore Long Island’s Map: Unique Regions & Insights - April 17, 2025