This article explores the trachealis muscle, a vital component of the respiratory system. We’ll delve into its anatomy, function, clinical significance, and ongoing research, aiming to provide a comprehensive understanding of this often-overlooked muscle.
Unveiling the Trachealis Muscle: A Respiratory Powerhouse
The trachealis muscle, a smooth muscle located on the posterior wall of the trachea, plays a crucial role in respiration. Its strategic location and dynamic action allow it to regulate airflow and protect the airway, making it a key player in respiratory health. [https://www.lolaapp.com/dorsogluteal-site]
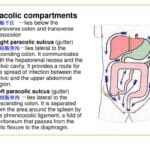
Location and Structure: Where Functionality Meets Form
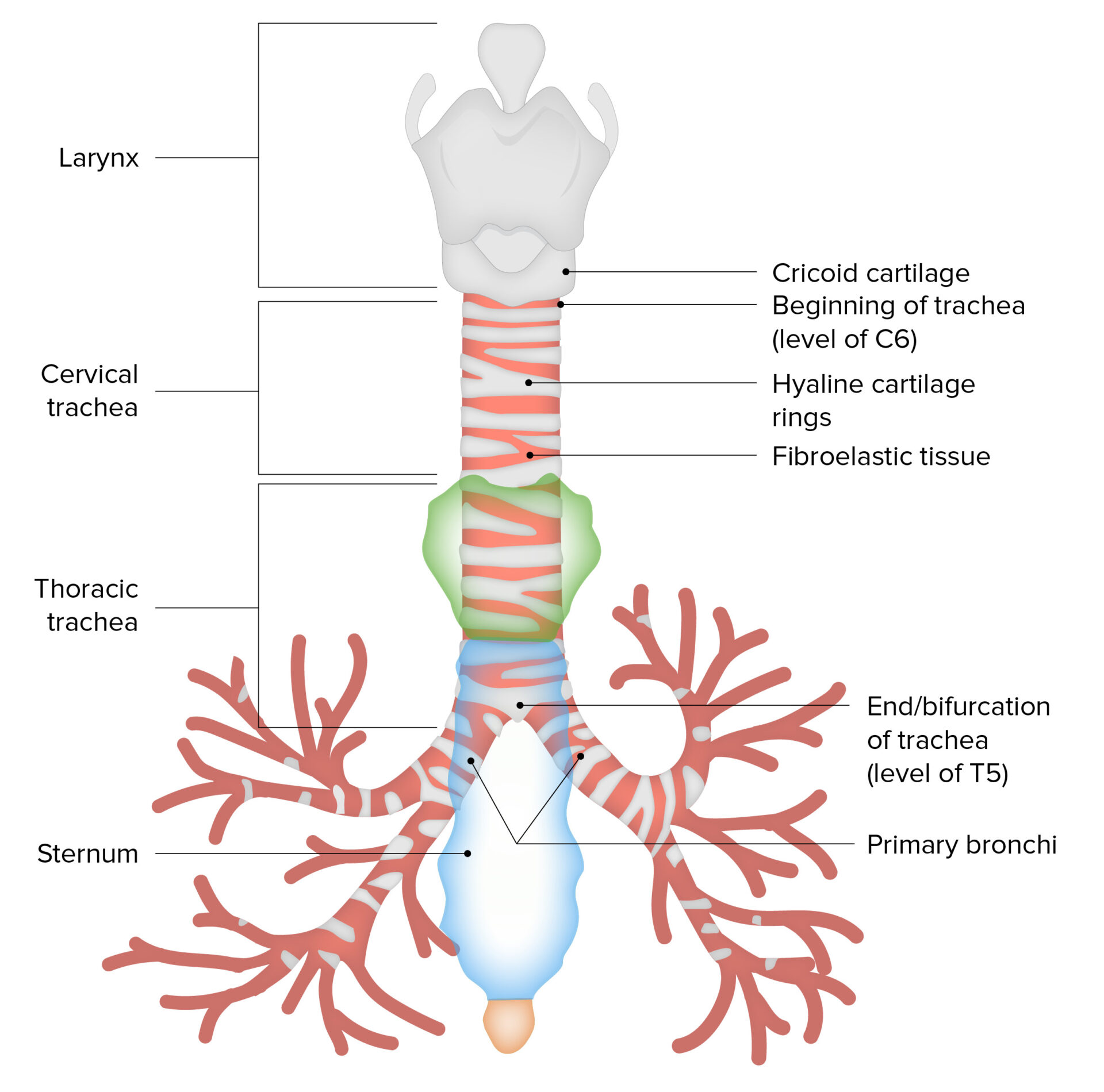
The trachea, commonly known as the windpipe, consists of C-shaped cartilage rings that provide structural support. The trachealis muscle spans the posterior gaps in these rings, completing the circular structure and forming the posterior wall of the trachea. This unique positioning, anterior to the esophagus, allows the trachealis to dynamically adjust the diameter of the trachea, influencing both breathing and swallowing. [https://www.lolaapp.com/gemellus-inferior]
The Trachealis in Action: Breathing, Coughing, and Swallowing
The trachealis muscle contributes to several essential functions:
- Airway Diameter Control: The trachealis muscle’s primary role is regulating airflow. By contracting, it narrows the trachea, increasing air velocity during coughing to expel mucus and foreign particles. Relaxation widens the trachea, enabling efficient airflow during normal breathing.
- Cough Mechanism: The forceful expulsion of air during a cough is largely due to the trachealis muscle’s contraction. This rapid narrowing of the trachea generates the necessary force to clear the airways.
- Swallowing Support: During swallowing, the trachealis muscle relaxes, allowing the trachea to narrow slightly and accommodate the expansion of the esophagus as food passes through. This coordinated action helps prevent food from entering the trachea.
Trachealis Muscle Dysfunction: Clinical Significance
When the trachealis muscle isn’t functioning correctly, it can contribute to various respiratory problems:
Tracheomalacia: A Concerning Weakness
Tracheomalacia, a condition where the trachea is abnormally soft and floppy, may involve hypotonia (weakness) of the trachealis muscle. This weakness can lead to tracheal collapse, especially during exhalation, causing breathing difficulties. Tracheomalacia is more common in infants and young children, but it can also affect adults.
Aging’s Impact: Stiffness and Reduced Elasticity
As we age, the trachealis muscle, like many other tissues, can lose elasticity and stiffen. This age-related change can decrease the trachea’s flexibility, potentially impacting respiratory function. Some studies suggest this stiffening might contribute to a decline in respiratory efficiency in older adults, particularly during exercise or times of respiratory stress.
Infant Intubation Challenges: Navigating a Tight Space
The trachealis muscle’s proximity to the esophagus can pose challenges during intubation, particularly in infants. The small size of the infant trachea and the close relationship between the trachea and esophagus increase the risk of tracheal compression if the endotracheal tube is positioned incorrectly. Careful intubation technique is crucial to avoid this complication.
The Trachealis Muscle: Current Research and Future Directions
While much is known about the trachealis muscle, ongoing research continues to explore its complexities:
- Neural Control: Researchers are investigating the precise mechanisms by which the nervous system controls the trachealis muscle’s contraction and relaxation, including the role of stretch receptors and their feedback mechanisms.
- Role in Respiratory Diseases: Studies are exploring the potential contribution of trachealis muscle dysfunction to various respiratory conditions beyond tracheomalacia, including asthma and COPD.
- Targeted Therapies: Scientists are exploring the possibility of developing targeted therapies to improve trachealis muscle function in individuals with tracheomalacia or other respiratory problems. This may involve medications, exercises, or other interventions.
- Evolutionary Significance: Comparative studies across species may offer clues about the trachealis muscle’s evolutionary history and adaptive significance, providing further insight into its function in humans.
Delving Deeper into Specific Questions
What is the trachealis muscle composed of?
The trachealis muscle is composed of smooth muscle tissue. This distinguishes it from skeletal muscles, which are under voluntary control. Smooth muscle operates involuntarily, allowing the trachealis to automatically adjust airway diameter without conscious effort.
When does the trachealis muscle contract during swallowing?
The trachealis muscle relaxes during swallowing, not contracts. This relaxation allows the trachea to constrict slightly, making room for the esophagus to expand as food passes through.
By continually exploring the intricacies of the trachealis muscle, researchers hope to uncover new strategies for diagnosing and treating respiratory conditions. This ongoing quest for knowledge underscores the importance of understanding even the smallest components of our respiratory system and their impact on overall health.
- Unveiling Bernhard Caesar Einstein’s Scientific Achievements: A Legacy in Engineering - July 15, 2025
- Uncover who is Jerry McSorley: CEO, Family Man, Business Success Story - July 15, 2025
- Discover Bernhard Caesar Einstein’s Scientific Contributions: Unveiling a Legacy Beyond Einstein - July 15, 2025




1 thought on “The Trachealis Muscle: Anatomy, Function, and Clinical Significance”
Comments are closed.