“The buzzing stopped, but the nightmare had just begun.” This chilling statement, echoing across online forums, captures the devastating reality for some individuals who sought relief from depression through Transcranial Magnetic Stimulation (TMS). While often touted as a safe and effective treatment, their experiences reveal a darker side, a landscape of debilitating side effects and shattered hopes. This investigative piece delves into the untold suffering of those for whom TMS not only failed to provide relief, but actively caused harm, raising critical questions about the hidden risks of this increasingly popular procedure.
The Unseen Scars of TMS: Stories of Suffering
The promise of TMS – a non-invasive alternative to medication – is undeniable. Yet, beneath the surface of optimistic projections lies a current of disquiet, fueled by the experiences of those who have been harmed. One Reddit user, after completing 40 TMS sessions, described a cascade of debilitating symptoms: seizures, crushing fatigue necessitating 12 hours of sleep per night, relentless headaches, vision changes, and a tragic worsening of the very depression TMS was meant to alleviate. “[TMS] ruined my life!” they wrote, a stark and desperate plea echoing the sentiments of others who feel abandoned by a system that promised healing. This isn’t an isolated incident. On platforms like Mad in America, similar stories emerge, painting a disturbing picture of lives disrupted, not healed, by TMS. “TMS not only has not improved my mental health but also has robbed me of some of the most important things in life,” one individual shared, their words a testament to the profound and lasting impact of TMS-induced harm. “Officially done with TMS and worse than when I started,” another lamented, a concise yet powerful indictment of a treatment gone wrong. These are not mere anecdotes; they represent a chorus of voices demanding recognition and raising serious questions about the true safety and efficacy of TMS.
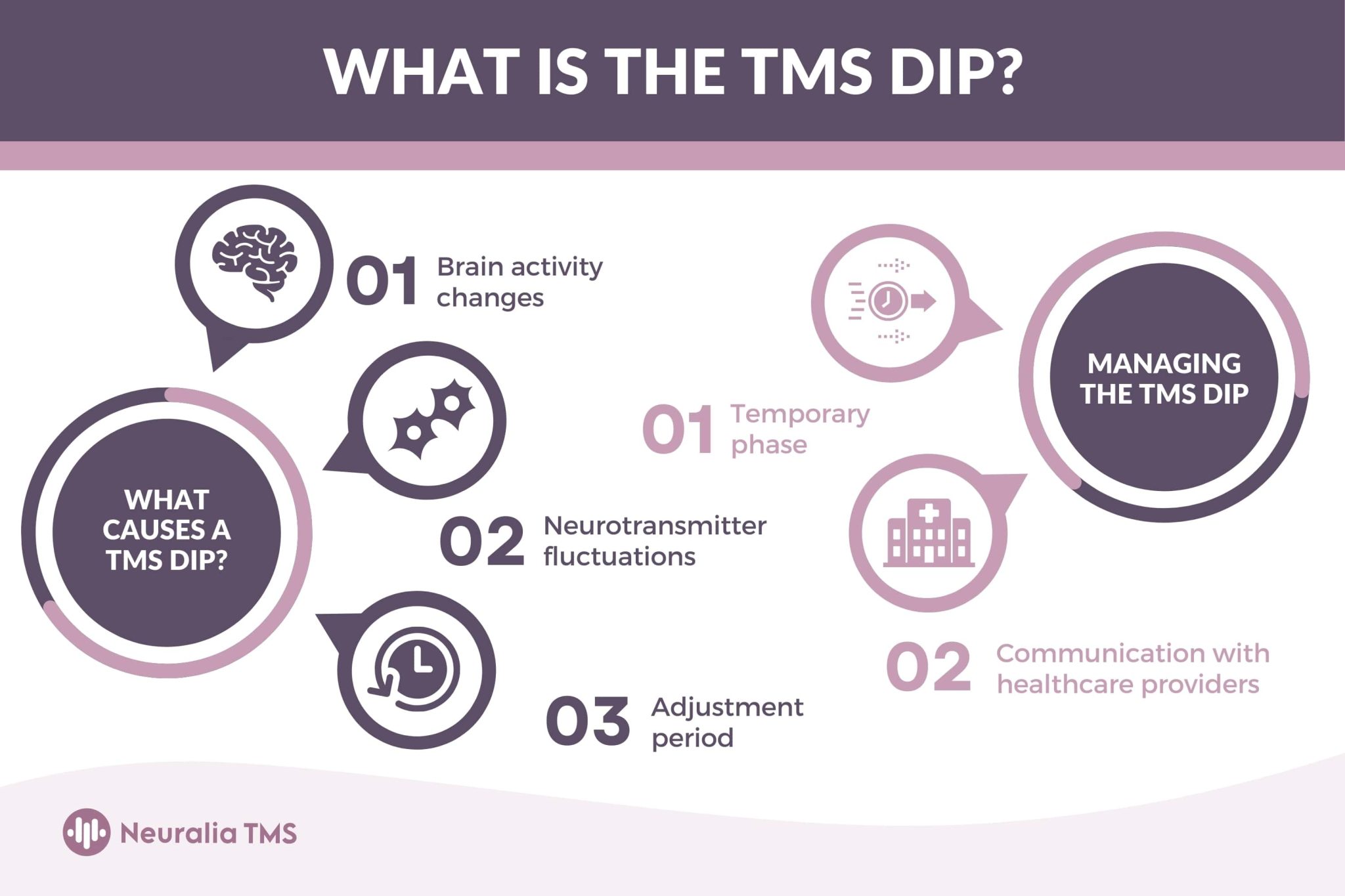
Unmasking the Risks: Beyond the Hype
While TMS undoubtedly holds potential, the limited research on long-term effects and the potential for severe neurological complications raises significant concerns. One commonly reported side effect, known as the “TMS dip,” involves a temporary intensification of symptoms. While often transient, for some, this “dip” becomes a persistent and devastating plunge into deeper despair, a cruel irony for those seeking solace from their mental health struggles (Source: madisonavetms.com, neuraliatms.com.au). The potential for seizures, though statistically rare, is a documented risk, underscoring the powerful neurological impact of TMS. Cognitive changes, including difficulties with memory, concentration, and other mental processes, have also been reported, raising troubling questions about the potential for long-term cognitive impairment. Are these risks being adequately communicated to patients? Are we truly grasping the long-term implications of this powerful technology?
Navigating the System: Misdiagnosis and Incomplete Treatment
The effectiveness of TMS is intrinsically linked to accurate diagnosis. Misdiagnosis, particularly in cases of bipolar disorder mistaken for major depression, can transform TMS from a potential solution into a source of further harm. In such instances, TMS may exacerbate symptoms, potentially triggering manic episodes and destabilizing an already fragile mental state (Source: revivalmentalhealth.com, neuraliatms.com.au). Prematurely discontinuing treatment, often due to unbearable side effects, can also have unintended negative consequences, potentially intensifying symptoms and leaving individuals feeling abandoned and hopeless (Source: neuraliatms.com.au). This raises crucial questions about the adequacy of current screening practices and the availability of support for those navigating the complexities of TMS treatment. Are we, as a medical community, doing enough to ensure proper diagnosis and comprehensive patient care?
A Call for Transparency and Accountability: Protecting Patients
The experiences of those harmed by TMS demand a critical reassessment of the current landscape. We need more research, more rigorous long-term studies, and, crucially, more support for those who have suffered adverse effects. Their stories, often dismissed or minimized, are indispensable pieces of the puzzle, offering invaluable insights into the complexities of TMS and informing its responsible and ethical application. How many more lives must be disrupted before we demand greater transparency and accountability from the TMS industry? Are we, as a society, adequately prioritizing patient well-being over profit? This is not about fear-mongering; it’s about advocating for patient safety and demanding better care. It’s about acknowledging the human cost of medical interventions and ensuring that the pursuit of innovation doesn’t come at the expense of individual well-being. The phrase “TMS ruined my life” is not merely a collection of words; it’s a cry for help, a plea for recognition, a demand for change. It’s a story we must heed.
The Uncertain Landscape of TMS Outcomes
The often-cited 50-60% success rate for treatment-resistant depression raises questions about the definition of “success” and the experiences of those who fall outside this statistic. Does “success” signify a modest improvement in mood or a complete remission of symptoms? What about the individuals who experience no benefit or, worse, suffer debilitating side effects? These questions underscore the complexity of evaluating TMS outcomes and the need for more nuanced reporting. Ever wondered about the immense wealth of Turki Al Sheikh? Uncover the details behind Turki Al Sheikh net worth and delve into the fascinating world of high finance.
The variability in individual responses to TMS highlights the need for personalized treatment plans. Factors such as the specific treatment protocol, the nature and severity of the underlying condition, and individual brain chemistry all likely play a role in determining treatment outcomes. A one-size-fits-all approach may not be the most effective strategy, and further research is needed to identify optimal treatment parameters for different patient populations. Are you curious about maximizing your financial potential? Discover the intricacies of what is a max funded IUL and unlock the secrets to a secure financial future. This underscores the importance of ongoing research, open communication between doctors and patients, and a cautious, individualized approach to TMS therapy.
Finally, the limited research on the long-term effects of TMS raises concerns about potential lasting neurological consequences. While TMS may offer hope for some, it’s essential to approach this treatment with realistic expectations and a clear understanding of both its potential and its limitations.
| Potential Side Effect | Description |
|---|---|
| Seizures | Sudden, involuntary electrical disturbances in the brain. |
| Fatigue | Overwhelming tiredness. |
| Headaches | Persistent or severe pain in the head. |
| Vision Changes | Alterations in eyesight. |
| Worsening Depression | An increase in the severity of depressive symptoms. |
| Cognitive Changes | Difficulties with memory, concentration, and other mental processes. |
This investigation is not intended to discourage the use of TMS but rather to advocate for greater transparency, more comprehensive research, and improved patient care. The stories of those who have suffered adverse effects must be heard and acknowledged. Only then can we ensure that the pursuit of innovative mental health treatments prioritizes patient safety and well-being above all else.
- Discover Long Black Pepper: Flavor & Health Benefits - April 25, 2025
- Shocking Twists: The Grownup Review: Unreliable Narration - April 25, 2025
- A Quiet Place Book vs Movie: A Deep Dive - April 25, 2025