Pseudobulbar affect (PBA) is a neurological condition characterized by involuntary outbursts of crying or laughing, often disproportionate to the situation. These episodes can be disruptive, impacting social interactions and quality of life. This comprehensive guide will explore PBA’s symptoms, causes, diagnosis, and management strategies, providing you with the information you need to navigate this challenging condition. A printable PBA information card is also included to help you explain PBA to others.
What is PBA?
PBA, sometimes referred to as emotional incontinence, is a neurological disorder marked by involuntary, inappropriate episodes of crying, laughing, or other emotional expressions. These outbursts are often exaggerated, exceeding the typical emotional response to a given situation. The disconnect between the emotion felt and the outward expression is a hallmark of PBA. For instance, someone with PBA might laugh uncontrollably at a funeral or sob during a joyous occasion. The frequency of these episodes, and the potential for rapid shifts from laughter to tears, further distinguishes PBA from typical emotional responses.
Imagine feeling overwhelmed by a sudden wave of tears during a business meeting or erupting in laughter at a somber occasion. These episodes aren’t intentional and can be utterly exhausting for those experiencing them. If the symptoms of depression or anxiety deteriorate or become unbearable with prednisone 5 day taper dose, then the patient must contact the doctor immediately. Also, the patient must not take any medication like physc to treat the depression on their own. PBA can significantly impact someone’s quality of life, making everyday interactions challenging and sometimes leading to social withdrawal.
Causes of PBA
PBA is a consequence of damage to the neural pathways in the brain that regulate emotional expression. This disruption can stem from various underlying neurological conditions, including:
- Stroke: Damage to brain tissue can interfere with emotional control.
- Traumatic Brain Injury (TBI): Injury to the brain can disrupt emotional regulation.
- Multiple Sclerosis (MS): Damage to the myelin sheath surrounding nerves can impair signal transmission, affecting emotional control.
- Amyotrophic Lateral Sclerosis (ALS; Lou Gehrig’s disease): Progressive degeneration of motor neurons can also impact emotional pathways.
- Alzheimer’s Disease: Brain cell deterioration affects various cognitive functions, including emotional regulation.
- Parkinson’s Disease: Changes in brain chemistry and function can contribute to PBA.
- Other Dementias: Cognitive decline can disrupt emotional control.
It’s important to note that while these conditions are associated with PBA, having one doesn’t guarantee you’ll develop the condition. Researchers are still exploring the intricacies of how these neurological conditions lead to emotional outbursts. Some theories suggest that the damage affects specific brain areas responsible for inhibiting emotional responses, while others propose that changes in brain chemicals play a crucial role.
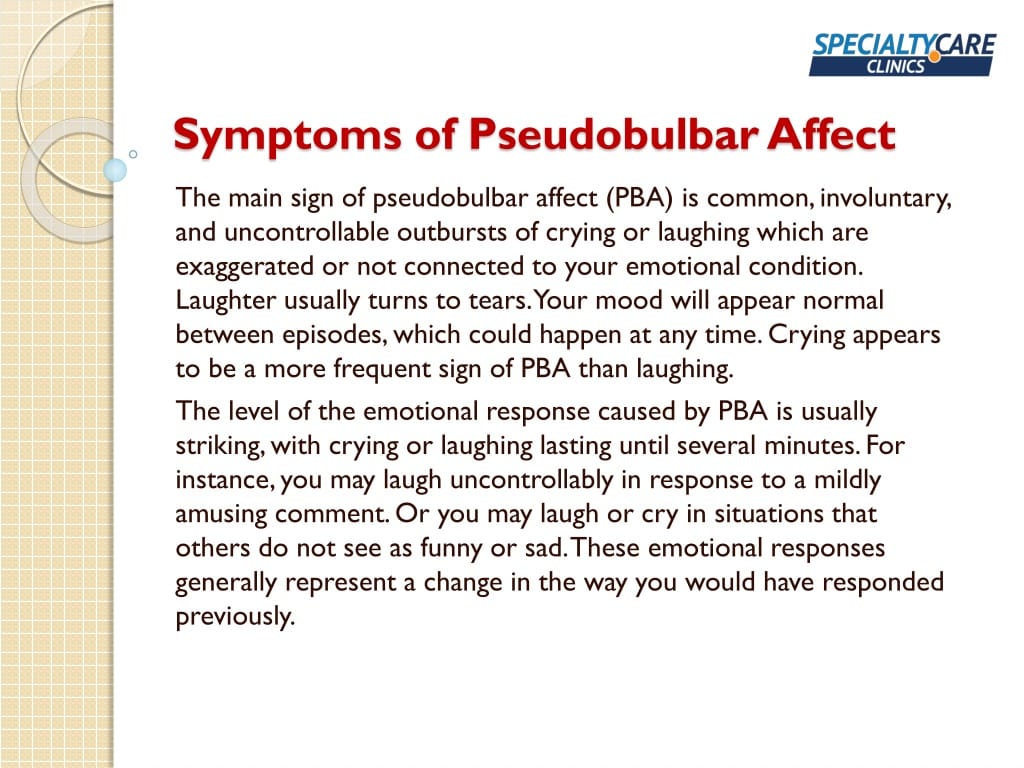
Recognizing PBA Symptoms
The primary symptoms of PBA are:
- Involuntary emotional outbursts: Sudden, uncontrollable episodes of crying or laughing.
- Exaggerated emotional responses: Reactions disproportionate to the situation.
- Inappropriate emotional displays: Laughing or crying at inappropriate times.
- Rapid shifts in emotion: Abrupt transitions between laughter and tears.
Diagnosing PBA
Diagnosing PBA involves a comprehensive evaluation, often by a neurologist or psychiatrist, to differentiate it from mood disorders like depression or bipolar disorder. This process includes:
- Neurological examination: Assessing medical history, symptoms, and underlying neurological conditions.
- Center for Neurologic Study-Lability Scale (CNS-LS): A questionnaire that quantifies the severity of PBA symptoms.
- Differential diagnosis: Distinguishing PBA from mood disorders by considering the sudden and involuntary nature of PBA episodes.
- Additional tests: Brain imaging (MRI or CT scan) and electroencephalography (EEG) may be used to rule out other conditions or identify underlying neurological issues.
Managing PBA
While there’s no cure for PBA, several management strategies can significantly improve symptoms and quality of life:
- Medication: Dextromethorphan hydrobromide and quinidine sulfate are FDA-approved for treating PBA. These medications may help reduce the frequency and intensity of emotional outbursts.
- Therapy: Cognitive behavioral therapy (CBT) can help individuals develop coping mechanisms to manage emotional responses and triggers.
- Support groups: Connecting with others experiencing PBA can provide emotional support and practical advice.
Living with PBA: Tips and Resources
PBA can significantly impact daily routines, relationships, and self-esteem. However, with proper diagnosis and treatment, individuals can regain a sense of normalcy and emotional well-being. Here are some additional tips for living with PBA:
- Develop coping strategies: Deep breathing exercises, mindfulness techniques, and distraction methods can help manage episodes when they arise.
- Build a strong support system: Connect with family, friends, and support groups to gain understanding and emotional support.
- Educate others about PBA: Raising awareness can reduce stigma and help others understand your experiences.
Printable PBA Information Card
This card summarizes key information about PBA and can be helpful for explaining the condition to others:
| Feature | Description |
|---|---|
| What is PBA? | A neurological condition causing involuntary emotional outbursts (laughing/crying). |
| Causes | Damage to brain pathways controlling emotions (stroke, MS, ALS, TBI, Alzheimer’s, Parkinson’s, etc.) |
| Symptoms | Involuntary crying/laughing, exaggerated emotional responses, rapid emotional shifts. |
| Diagnosis | Based on symptoms, neurological examination, and sometimes brain imaging (MRI). |
| Treatment | Medication (e.g., dextromethorphan/quinidine), therapy (e.g., CBT), support groups. |
This information is intended for educational purposes only and should not be considered medical advice. Always consult with a healthcare professional for any health concerns or before making any decisions related to your health or treatment.
- China II Review: Delicious Food & Speedy Service - April 17, 2025
- Understand Virginia’s Flag: History & Debate - April 17, 2025
- Explore Long Island’s Map: Unique Regions & Insights - April 17, 2025