This article explains periodontal staging and grading, essential tools for understanding and managing gum disease. We’ll explore what these terms mean, why they’re important for your oral health, and how they guide treatment decisions.
Decoding Gum Disease Severity
Dentists use periodontal staging and grading to assess the severity and predict the progression of gum disease. Staging measures the current damage, while grading forecasts how quickly the disease might worsen.
Staging: Assessing the Damage
Staging evaluates the existing damage caused by gum disease, similar to assessing damage after a storm. It measures how much the gums and supporting bone have been affected. Key measurements include:
- Clinical Attachment Loss (CAL): Measures how much the gums have receded from the teeth. This is a primary indicator of disease severity. Greater recession suggests more advanced periodontitis.
- Probing Depth: A small probe measures the depth of the pockets between your gums and teeth. Deeper pockets usually indicate more advanced disease.
- Bone Loss: X-rays reveal how much bone supporting the teeth has been lost.
- Tooth Loss: In advanced stages, tooth loss is a significant factor in determining the stage.
- Complexity Factors: This includes additional complications like furcation involvement (bone loss between the roots), loose teeth, or bite changes.
There are four stages, ranging from Stage I (early, minimal damage) to Stage IV (advanced, significant damage). The higher the stage, the more extensive the damage.
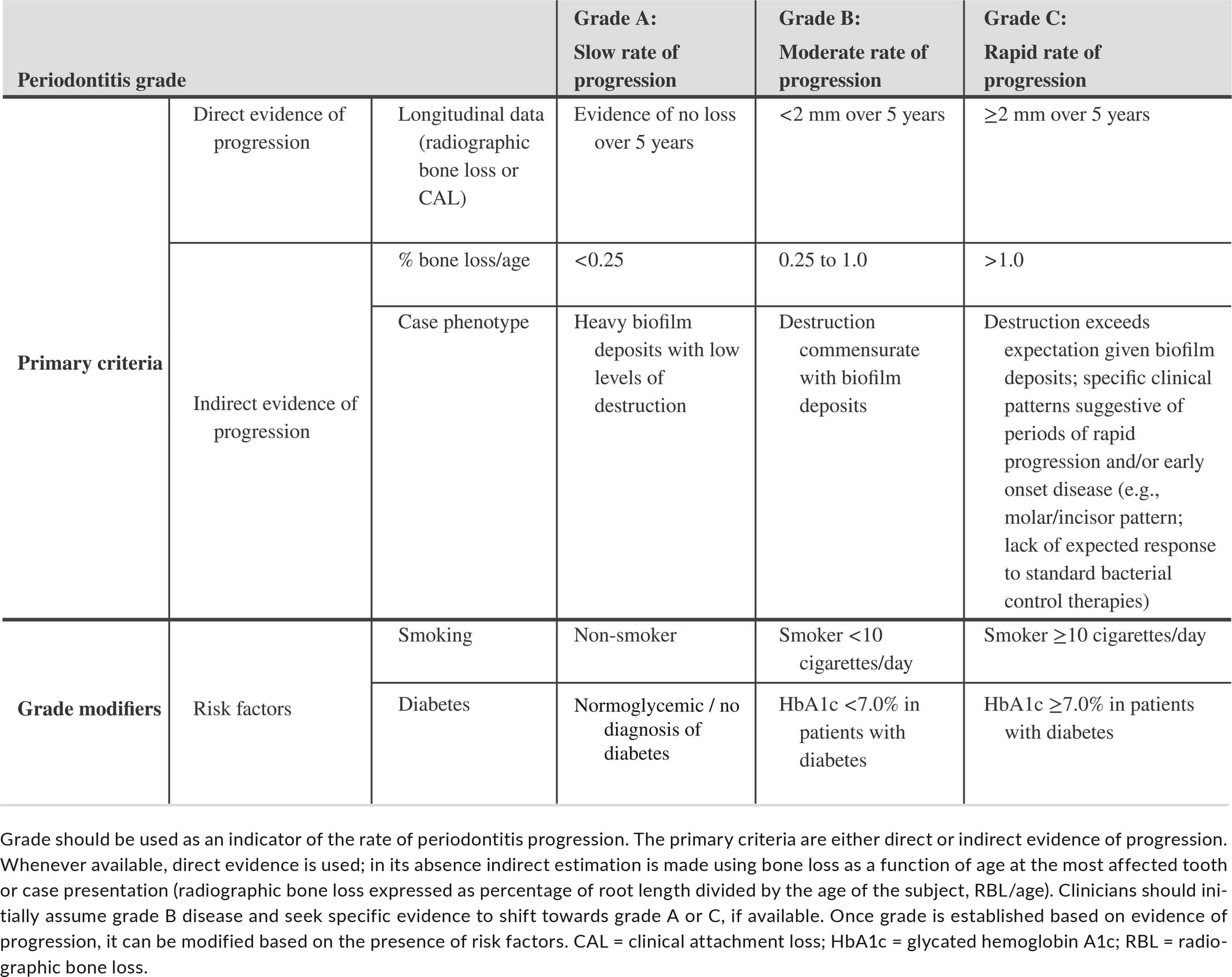
Grading: Forecasting the Future
Grading predicts the likely progression of gum disease and identifies contributing factors. It’s like a weather forecast, considering:
- Progression Rate: How quickly the disease is advancing (slow, moderate, or rapid).
- Risk Factors: Factors like smoking, diabetes, genetics, stress, and poor oral hygiene that might accelerate disease progression.
- Systemic Health Impact: How periodontitis might be affecting your overall health. For example, some experts believe there’s a correlation between gum disease and heart disease. Research continues to explore these connections. Removal of a PICC line may also be relevant in cases where systemic infections are a concern.
Grading helps dentists determine the likelihood and speed of disease progression, essential for developing a personalized treatment plan.
The 2018 Classification System: A Comprehensive Approach
The 2018 classification system combines staging and grading for a more thorough evaluation. It addresses the paradox where tooth loss due to gum disease could appear to improve staging, even though the overall condition remains serious. This system provides a more accurate and dynamic assessment, considering changes over time.
Why Understanding Staging and Grading Matters
Understanding these concepts empowers you to actively participate in your oral health:
- Understand Your Condition: Staging and grading clarify the extent and potential impact of your gum disease.
- Communicate with Your Dentist: It equips you to ask informed questions and discuss treatment options. For instance, if you’re a candidate for perianesthesia, understanding staging and grading can help you discuss the process with your dentist. If you’re interested in learning how to handle a patient that requires perianesthesia, click here.
- Make Informed Decisions: You can make educated decisions about your care and choose the best approach for your individual needs.
- Improve Your Prognosis: Understanding the factors influencing your gum disease enables you to make lifestyle changes and follow treatment recommendations, ultimately improving your chances of successful treatment.
What is Staging and Grading of Periodontitis?
Periodontitis, commonly known as gum disease, is a severe infection damaging the soft tissues and bone supporting your teeth. Staging and grading are essential for diagnosis and treatment.
Sizing Up the Damage: Staging
Staging assesses the current extent of the damage. It considers:
- Clinical Attachment Loss (CAL): Measures how far the gums have receded from the teeth.
- Bone Loss: X-rays help determine the extent of bone loss.
- Tooth Loss: A major factor in staging, as tooth loss is a common consequence of advanced periodontitis.
- Complexity Factors: Additional issues like furcation involvement, loose teeth, or bite changes.
Predicting the Future of Your Gums: Grading
Grading predicts the likely speed of disease progression. Factors include:
- Progression Rate: How fast the disease is advancing, based on past records or current assessments.
- Risk Factors: Smoking, diabetes, genetics, and stress can influence progression.
- Overall Health Impact: The effect of periodontitis on overall well-being.
Why Does Staging and Grading Matter?
Staging and grading are crucial for:
- Personalized Treatment: Tailoring treatment to your specific needs.
- Predicting the Path: Anticipating the course of the disease and adjusting treatment accordingly.
- Clear Communication: Providing a standardized language for dental professionals.
- Tracking Progress: Monitoring treatment effectiveness and making necessary adjustments.
| Feature | Staging | Grading |
|---|---|---|
| Focus | Current extent of damage | Likely future progression |
| Key Factors | CAL, bone loss, tooth loss, complexity factors | Progression rate, risk factors, overall health impact |
| Purpose | Assess severity and tailor treatment | Predict disease course and adjust treatment as needed |
How Do You Calculate Periodontal Grading?
Periodontal grading predicts how quickly gum disease may progress. It involves analyzing X-rays for bone loss, considering age, and other risk factors. Age and bone loss are significant indicators; younger individuals with substantial bone loss may suggest a more aggressive disease form.
The formula for calculating periodontal grade is:
Periodontal Grade = Highest Percentage of Bone Loss / Patient’s Age
This calculation categorizes the likely progression:
- Grade A (Slow Progression): Minimal risk factors, slow progression.
- Grade B (Moderate Progression): One or more risk factors, moderate progression.
- Grade C (Rapid Progression): Multiple risk factors, potentially rapid progression.
Risk Factors:
- Smoking: Impairs blood flow to gums, hindering healing.
- Diabetes: High blood sugar weakens immune response.
- Genetics: Predisposition to gum disease.
- Stress: Weakens the immune system.
- Poor Oral Hygiene: Allows bacteria to thrive.
Ongoing research continues to refine our understanding of periodontal disease. Remember, this grading system is a tool, and a comprehensive dental exam and health history are essential for accurate assessment.
Perio Stage 3 vs. Stage 4: Understanding the Critical Differences
Understanding the differences between Stage 3 (severe) and Stage 4 (advanced) periodontitis is crucial for effective treatment.
Stage 3 involves increased gum recession, persistent bad breath, and possible tooth mobility. Some individuals may experience pain while chewing.
Stage 4 exhibits significant bone loss, leading to very loose teeth, potential tooth loss, and bite changes. Chewing becomes difficult, and the infection may impact overall health.
Here’s a comparison:
| Feature | Stage 3 Periodontitis | Stage 4 Periodontitis |
|---|---|---|
| Severity | Severe | Very Severe/Advanced |
| Bone Loss | Moderate | Major, up to 50% or more |
| Tooth Mobility | Possible, teeth may start to loosen | Significant, teeth very loose, may fall out |
| Gum Recession | Noticeable | Severe |
| Treatment | Often non-surgical options available | Usually requires surgery |
Treatment for Stage 3 often involves non-surgical methods like deep cleaning and antibiotics. However, Stage 4 typically requires surgical intervention due to significant bone loss. This might include flap surgery, bone grafting, or guided tissue regeneration. In some cases, extraction becomes necessary, followed by tooth replacement options.
Early detection and treatment are crucial. Regular dental check-ups are vital for identifying gum disease in its early stages when it’s more manageable. Contact your dentist if you notice any signs like bleeding gums, redness, swelling, or persistent bad breath.







1 thought on “Understanding Periodontal Staging and Grading: A Guide to Diagnosis and Treatment”
Comments are closed.