Got a sore, swollen, and infected flap of gum hanging over your wisdom tooth? You likely have pericoronitis, a common issue when wisdom teeth struggle to erupt. Operculectomy, a minor surgical procedure to remove this troublesome gum flap, offers a solution. This comprehensive guide covers everything you need to know about operculectomy—what it is, why you might need it, the procedure itself, recovery, potential complications, and alternatives. We’ll also delve into frequently asked questions to equip you with the knowledge you need to make informed decisions about your oral health.
Understanding Operculectomy
Have you noticed a flap of gum tissue partially covering your wisdom tooth? That’s the operculum. Sometimes, this flap can become infected and painful, a condition called pericoronitis. Operculectomy is the surgical removal of this flap.
What is it?
Operculectomy is a minor surgical procedure where the operculum, the excess gum tissue covering a partially erupted tooth (most often a wisdom tooth), is removed. It’s a relatively common and straightforward procedure.
Why might you need it?
The operculum can trap food and bacteria, leading to pericoronitis, characterized by swelling, pain, redness, and difficulty opening your mouth. Operculectomy helps prevent and treat pericoronitis by removing the source of the problem, improving oral hygiene, and protecting surrounding teeth.
The Operculectomy Procedure
An operculectomy is typically quick and performed under local anesthetic in a dental office or oral surgery clinic. You’ll be awake but shouldn’t feel pain, just some pressure.
- Anesthesia: The area is numbed.
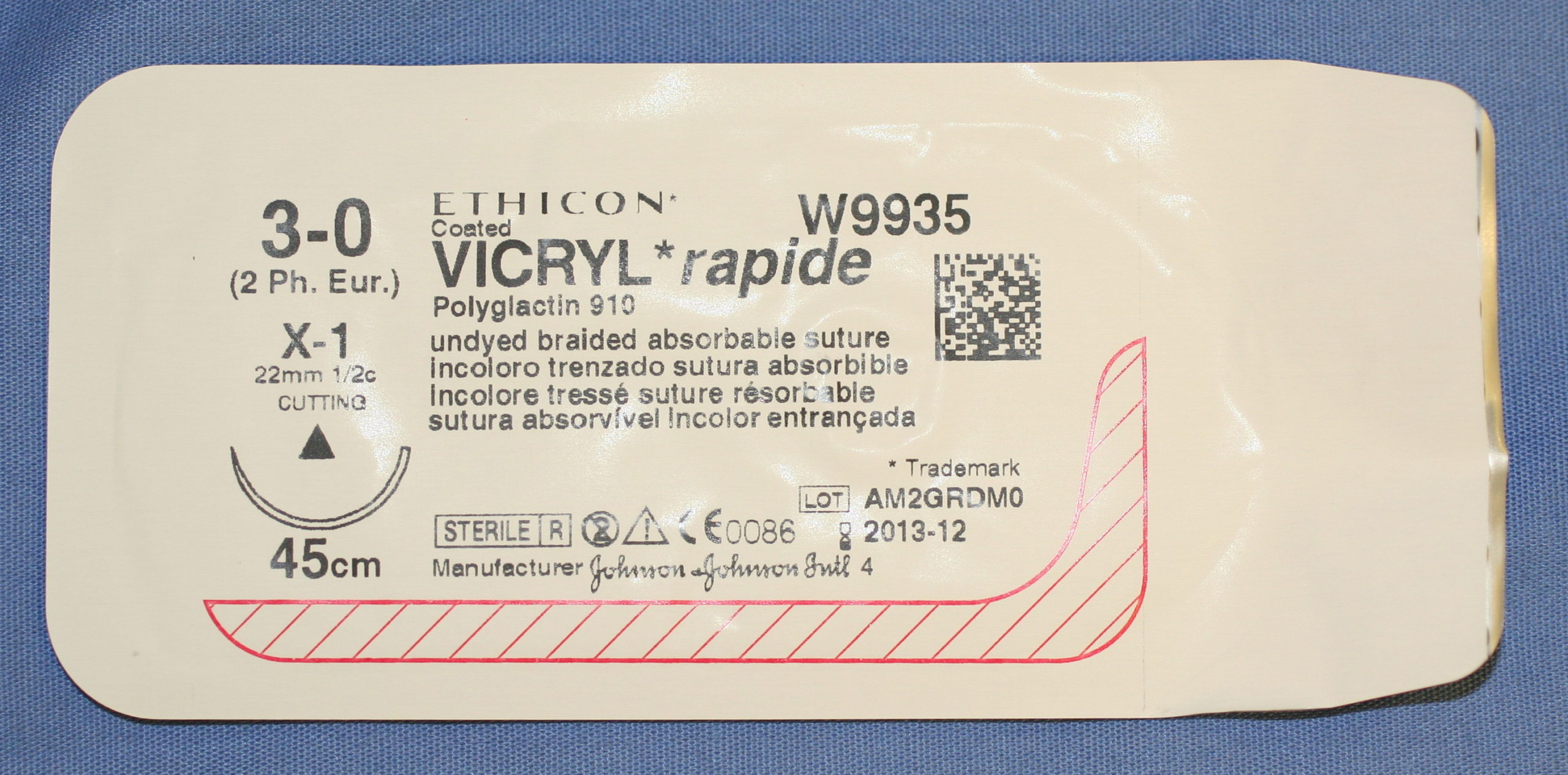
- Removal: The operculum is excised using a scalpel or, increasingly, a laser. Some early research suggests laser operculectomy [https://www.lolaapp.com/] may offer benefits like faster healing and less post-operative pain, though more research is ongoing.
- Cleaning and Sutures: The area is cleaned, and stitches may be placed.
Recovery and Aftercare
After your operculectomy, expect some soreness and swelling. Managing post-operative care is crucial for optimal healing and minimizing complications.
What to Expect
- Pain Management: Over-the-counter pain relievers (ibuprofen, acetaminophen) usually suffice. Stronger medication can be prescribed if needed. Ice packs can also help reduce swelling in the first 24 hours.
- Oral Hygiene: Rinse gently with warm salt water several times daily. Avoid vigorous brushing or rinsing near the surgical site initially.
- Diet: Stick to soft foods (yogurt, soup, scrambled eggs) for a few days.
- Activity: Avoid strenuous activities initially.
Healing Timeline
Recovery varies, but here’s a general guideline:
| Healing Stage | Timeframe | What to Expect |
|---|---|---|
| Initial Healing | 7-10 days | Reduced pain, swelling, and discomfort. You can likely resume most normal activities. |
| Complete Healing | Several weeks (up to a month or more) | Full gum tissue regeneration and resolution of tenderness. |
Several factors influence healing: overall health, adherence to post-op instructions, and procedure complexity.
Potential Risks and Complications
While generally safe, operculectomy carries potential risks, though rare:
- Bleeding, Infection, Dry Socket: Standard surgical risks.
- Lingual Nerve Damage: A small risk of damage to the lingual nerve, potentially causing temporary or permanent numbness or altered sensation in the tongue, lower lip, or chin.
- Operculum Regrowth: While uncommon, it’s a possibility.
Operculectomy vs. Extraction
Sometimes, extraction (removal of the entire tooth) is necessary. Here’s a comparison:
| Feature | Operculectomy | Extraction |
|---|---|---|
| Purpose | Removes excess gum tissue | Removes the entire tooth |
| Invasiveness | Less invasive | More invasive |
| Recovery Time | Shorter | Longer |
| Cost | Typically lower | Typically higher |
| Long-Term Solution | May not be permanent; extraction might still be needed | Usually a definitive solution |
Your dentist will determine the best approach based on your individual situation.
When to Call Your Dentist
Contact your dentist immediately if you experience:
- Persistent or worsening pain
- Excessive bleeding or swelling
- Signs of infection (pus, fever)
Frequently Asked Questions
- Cost: Varies based on location, complexity, and insurance. Your dental office can provide an estimate.
- Insurance Coverage: Many plans cover at least partially, especially if medically necessary. Check with your provider for specifics.
- Finding a Qualified Professional: Your dentist can refer you to an oral surgeon or periodontist.
Does the Gum Grow Back?
The original operculum doesn’t regenerate. However, the surrounding gum tissue heals and forms a new gumline. This process usually takes several weeks.
Operculectomy addresses the infected tissue, but underlying issues, like an impacted tooth, may require further treatment, like extraction. Ongoing research explores factors influencing gum healing and potential new techniques for tissue regeneration.
Long-Term Implications and Alternatives
If issues persist after operculectomy, or if the tooth is significantly impacted, your dentist probably will suggest extraction, especially with wisdom teeth that lack sufficient eruption space. Some experts believe leaving partially erupted teeth can lead to recurring problems. While antibiotics and improved oral hygiene may manage pericoronitis in some cases, operculectomy or extraction often provides a more definitive solution for long-term oral health.
Delve into the potential implications of extended Sermorelin usage by exploring the documented sermorelin long term side effects.
- China II Review: Delicious Food & Speedy Service - April 17, 2025
- Understand Virginia’s Flag: History & Debate - April 17, 2025
- Explore Long Island’s Map: Unique Regions & Insights - April 17, 2025