Imagine nursing as a puzzle, with each patient a unique set of pieces. Maslow’s Hierarchy of Needs acts as your guidebook, revealing the diverse needs patients have, from basic survival to self-fulfillment. By understanding this hierarchy, nurses can provide care that addresses not only physical ailments but also promotes holistic well-being and preserves patient dignity. Learn more about Maslow’s hierarchy of needs and nursing.
Decoding Patient Needs with Maslow’s Hierarchy
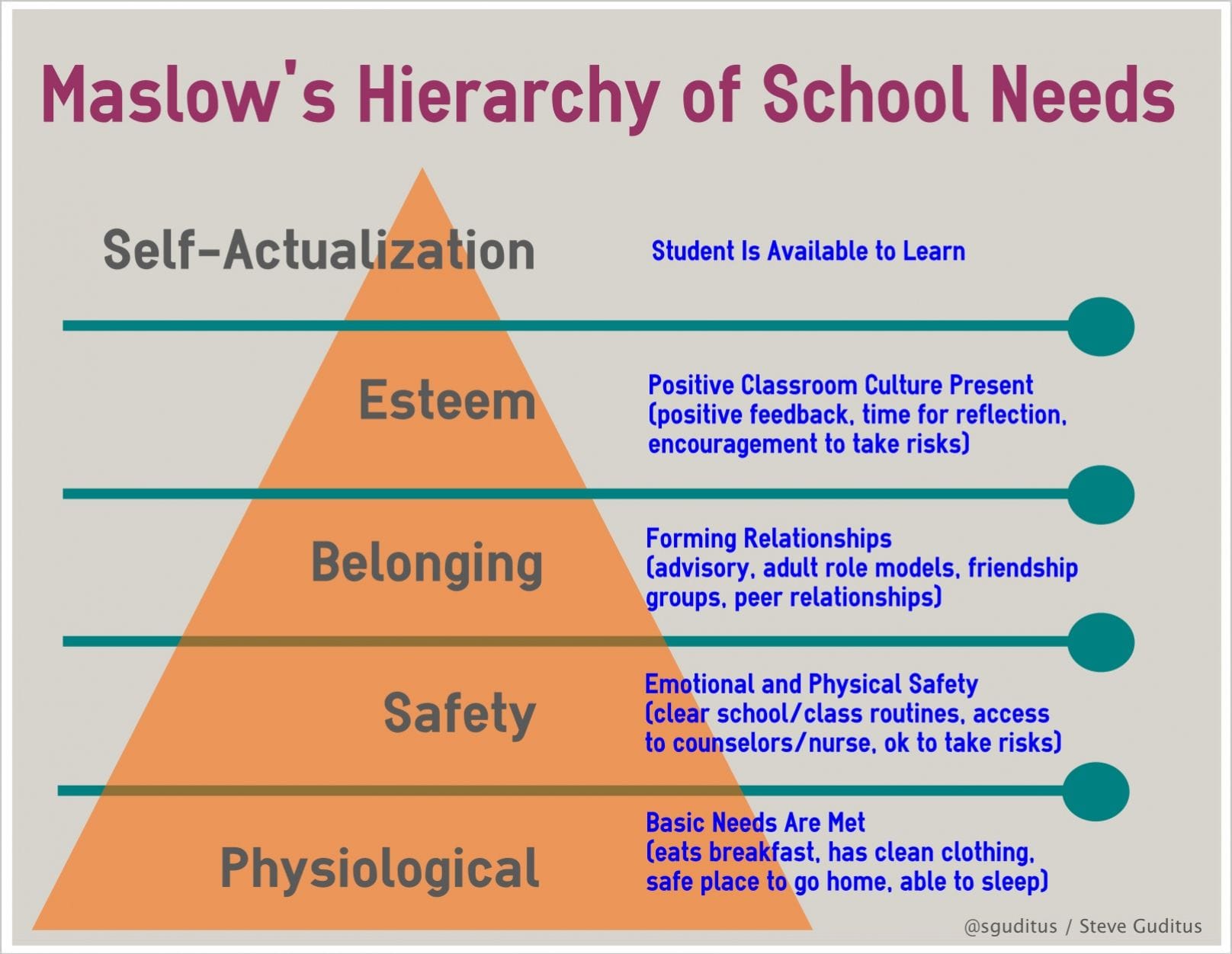
Maslow’s Hierarchy of Needs is a fundamental concept in psychology crucial for nurses aiming to provide holistic care and succeed on the NCLEX-RN. It suggests that human needs are hierarchical, like a pyramid. Just as you can’t build a roof before the foundation, higher-level needs become relevant only after addressing the foundational ones.
Understanding the Five Levels of Needs
Maslow’s Hierarchy outlines five key levels:
Physiological Needs: The absolute essentials for survival—breathing, food, water, sleep, shelter, and stable body temperature.
Safety Needs: Once physiological needs are met, safety and security become paramount. This includes physical safety, financial stability, and a predictable environment.
Love and Belonging Needs: This level focuses on social connections—love, affection, intimacy, and belonging within family, friendships, and community.
Esteem Needs: This encompasses self-esteem, confidence, achievement, respect, and a sense of accomplishment.
Self-Actualization Needs: The peak of the pyramid, representing the drive to reach full potential through personal growth, creativity, and finding purpose.
Applying Maslow’s Hierarchy to Nursing Practice
Maslow’s Hierarchy serves as a roadmap for nurses, helping prioritize patient needs. For example, a patient struggling to breathe needs oxygen before addressing emotional concerns.
Putting the Hierarchy into Action: A Step-by-Step Guide
Assessment: Carefully observe your patient, gather information through conversations and medical history, and identify unmet needs within Maslow’s framework.
Prioritization: Determine the most pressing needs. Remember, physiological needs typically come first. A high fever demands immediate attention, possibly preceding psychological needs.
Intervention: Develop and implement a care plan to address prioritized needs. This may involve administering medication, providing emotional support, or coordinating with other healthcare professionals.
Evaluation: Assess intervention effectiveness. Is the patient’s condition improving? Are their needs being met? Adjust the care plan as needed.
Maslow’s Hierarchy and the NCLEX-RN
The NCLEX-RN frequently tests your understanding of Maslow’s Hierarchy through patient scenarios requiring prioritized care based on these principles. Mastering this framework is crucial for exam success.
Maslow’s Hierarchy for Nurses: Self-Care Matters
Maslow’s Hierarchy applies to nurses too! Unmet personal needs, like exhaustion and lack of support, hinder providing compassionate care. Self-care is vital for both personal and professional well-being.
Looking Ahead: Nuances and Ongoing Research
Maslow’s hierarchy is a valuable guide, but it isn’t absolute. Cultural factors, individual differences, and circumstances can influence how needs are prioritized. Ongoing research explores these nuances and the complex interplay of needs, suggesting the hierarchy may not always be fixed. Additionally, research is exploring the connection between unmet needs in nurses and the risk of burnout.
Key Points of Maslow’s Hierarchy of Needs for Nurses:
- Five Levels of Needs: Physiological, Safety, Love and Belonging, Esteem, Self-Actualization.
- Foundation Approach: Address lower-level needs before higher ones.
- Holistic Care: Consider all levels of a patient’s needs.
- Prioritization Guide: Use the hierarchy to prioritize patient care.
- Step-by-Step Process: Assess, prioritize, intervene, and evaluate.
- NCLEX-RN Relevance: Essential for exam success.
- Self-Care for Nurses: Apply the hierarchy to personal well-being.
- Cultural and Individual Variations: Recognize that needs may vary.
- Ongoing Research: Our understanding continues to evolve.
Maslow in Action: Real-World Examples for Nurses
Now, let’s explore how nurses apply Maslow’s Hierarchy in everyday practice. This framework helps provide truly holistic, patient-centered care.
Addressing Each Level of the Pyramid
The Foundation: Physiological Needs: These are the non-negotiables for survival. Nurses ensure patients receive adequate nutrition, hydration, oxygen, rest, and a comfortable temperature.
Building Security: Safety Needs: This involves physical safety (preventing falls, infections) and emotional security (creating stability, explaining procedures clearly).
Connection and Support: Love and Belonging Needs: Nurses facilitate connections with loved ones, foster a sense of belonging, and offer emotional support, preventing isolation.
Building Confidence: Esteem Needs: Nurses involve patients in care decisions, praise efforts, and help them feel a sense of accomplishment, boosting self-esteem.
Reaching Full Potential: Self-Actualization Needs: Even in a healthcare setting, nurses can support self-actualization by encouraging realistic goals, providing resources for interests, and helping patients maintain a sense of purpose.
Navigating Nuances and Uncertainties
Maslow’s hierarchy isn’t a rigid checklist. Human needs are complex. A patient might prioritize seeing family (love/belonging) even before a lower need is fully met. Nurses use judgment, experience, and patient input to determine the most pressing needs, recognizing that research suggests the hierarchy can vary based on individual and cultural factors. Furthermore, ongoing research on human motivation and needs continues to evolve our understanding, emphasizing the importance of flexibility in patient care.
Maslow’s Hierarchy: The Foundation of Nursing Care
We’ve already discussed how Maslow’s Hierarchy guides patient care, but how exactly does it translate to the basic needs theory in nursing? It all starts with recognizing that sometimes, the simplest things have the greatest impact.
Understanding the Five Core Needs
Maslow proposed that everyone has these five core needs:
Physiological Needs: Survival essentials. Nurses prioritize ensuring patients have adequate oxygen, fluids, pain management, and comfortable rest.
Safety Needs: This involves physical and emotional safety. Nurses provide clear information, a calm environment, and access to support systems, easing patient anxieties.
Love and Belonging Needs: Nurses encourage visits, facilitate communication, and offer compassionate support, combating loneliness and promoting healing.
Esteem Needs: Nurses acknowledge patient strengths, encourage independence, and celebrate progress, fostering self-esteem during illness.
Self-Actualization Needs: While not always the immediate focus, nurses can support self-actualization by encouraging expression, respecting values, and helping patients find meaning amidst health challenges.
| Need Level | Description | Nursing Considerations |
|---|---|---|
| Physiological | Basic survival requirements | Providing food, water, comfortable temperature, pain relief |
| Safety | Security, stability, protection | Ensuring a safe environment, emotional support, clear communication |
| Love/Belonging | Connection, relationships, community | Facilitating visits, communication with family, building rapport |
| Esteem | Self-respect, confidence, achievement | Encouraging independence, celebrating progress, positive reinforcement |
| Self-Actualization | Reaching full potential, personal growth | Supporting personal goals, respecting values, finding meaning |
Maslow’s theory is a guideline, not a rigid rule. Sometimes, higher-level needs take precedence. Ongoing research suggests these needs can interact in more complex ways than originally thought. However, it reminds us that patient-centered care involves understanding the individual and what matters most to them.
Prioritizing Patient Care: A Step-by-Step Guide with Maslow
Now, let’s break down how nurses precisely prioritize patient care using Maslow’s Hierarchy of Needs. It’s all about building from the foundation up, addressing fundamental needs before moving toward self-fulfillment.
Applying the Hierarchy in Practice
Physiological Needs: The Foundation: Focus on breathing, fluids, nutrition, rest, and temperature regulation.
Safety and Security: Building the Walls: Implement fall precautions, manage pain and anxiety, and ensure a secure, caring environment.
Love and Belonging: Adding the Doors and Windows: Build rapport, encourage visits from loved ones, and facilitate social interaction.
Esteem Needs: Furnishing the House: Recognize patient strengths, encourage independence, and celebrate achievements, however small.
Self-Actualization: Making it a Home: Encourage exploration of interests, provide resources for personal growth, and respect individual values.
Practical Application and Prioritization
A patient struggling to breathe demands immediate attention above all else. Once the patient is stable, then addressing other needs like social interaction becomes appropriate. It’s important to remember that Maslow’s hierarchy, while valuable, isn’t inflexible. Research suggests variations in the order of needs based on individual and cultural factors. This framework, used with critical thinking and patient input, ensures comprehensive and compassionate care, addressing both physical ailments and overall well-being.















1 thought on “Maslow’s Hierarchy of Needs: A Practical Guide for Nurses and NCLEX-RN Success”
Comments are closed.