Obstructive sleep apnea (OSA) disrupts sleep with pauses in breathing, impacting overall health and quality of life. Nasopharyngeal stents offer a minimally invasive alternative to CPAP for some OSA sufferers, improving nasal airflow and reducing snoring. This article explores nasopharyngeal stents—their types, effectiveness, benefits, risks, and patient experiences—to provide a comprehensive understanding of this treatment option. Learn more about the innovative OMG approach to understanding nasopharyngeal stents. For more information on related medical systems, check out the medical systems test menu.
What are Nasopharyngeal Stents?
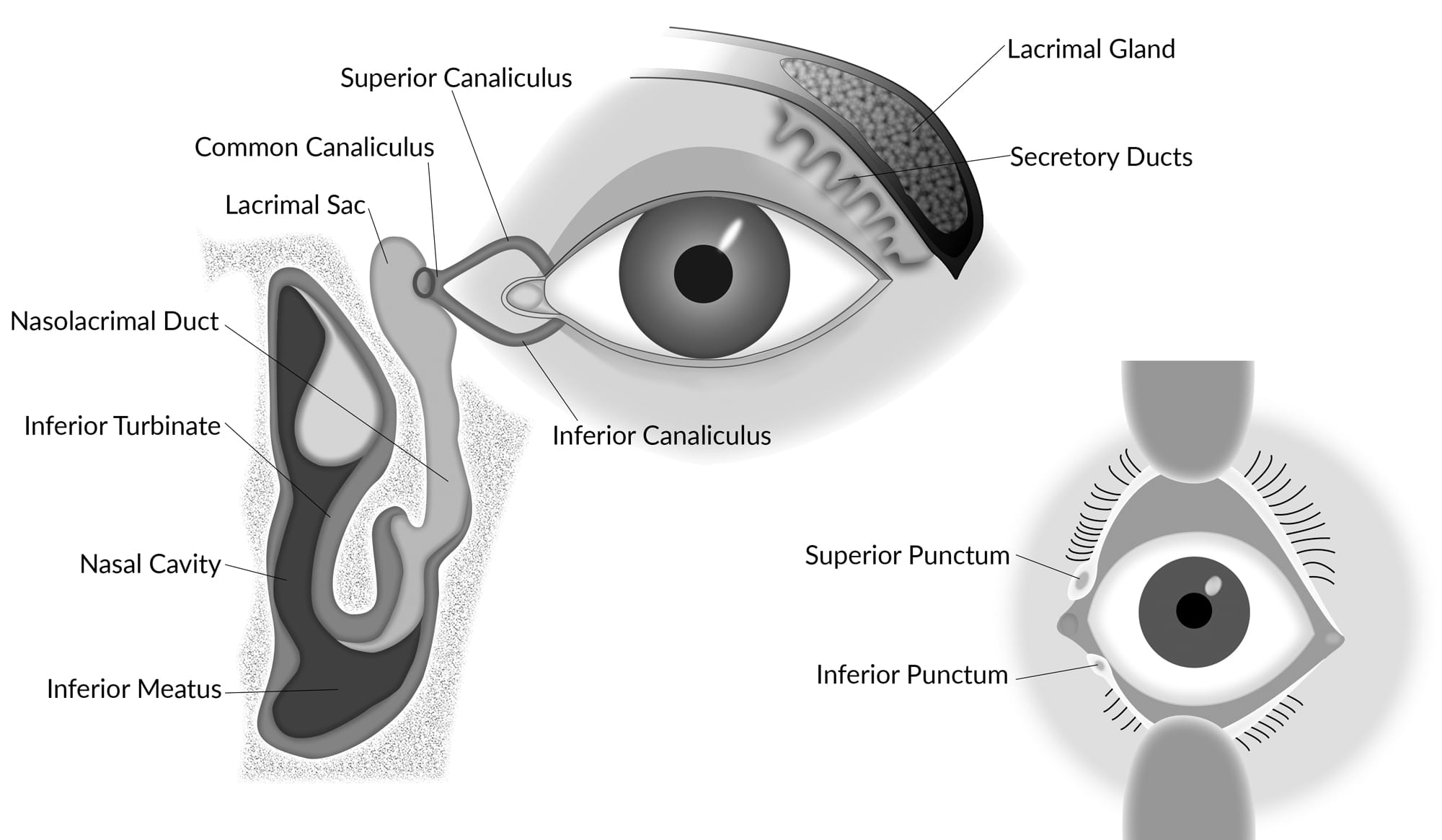
Nasopharyngeal stents are small, flexible devices inserted into the nasal passages to help maintain an open airway. They are primarily used to treat obstructive sleep apnea (OSA) and snoring. These stents act like tiny scaffolds, gently widening the nasal passages to reduce airflow resistance, making it easier to breathe, especially during sleep. While CPAP therapy remains a highly effective treatment for OSA, some individuals find it difficult to tolerate. Nasopharyngeal stents may provide a less cumbersome alternative for select patients.
Types of Nasopharyngeal Stents
Nitinol and silicone are the primary materials used in nasopharyngeal stents, each with unique properties affecting comfort and functionality. The choice of stent depends on factors like the severity of OSA and individual nasal anatomy. Your doctor will help determine the most suitable option.
- Nitinol Stents (e.g., AlaxoStent): These self-expanding stents are made from nitinol, a flexible metal alloy with shape memory. Compressed for insertion, they gently expand within the nasal passage to maintain its openness. A 2022 NCBI study explored the therapeutic use of the AlaxoStent.
- Silicone Stents (e.g., Nastent): These pre-formed silicone tubes are inserted directly into the nasal passages. Studies published in PubMed (2022), Oxford Academic (2018), and Karger Publishers (2020) have evaluated the therapeutic effects and diagnostic value of silicone stents like Nastent, specifically their efficacy in maintaining nasal airway patency and treating mild-to-moderate OSA.
- Nasal Trumpets: Shorter and less invasive than stents, nasal trumpets are typically used for short-term relief after nasal surgery or for specific conditions. They resemble small tubes and help maintain open nasal passages.
How Effective Are Nasopharyngeal Stents?
Studies on nasopharyngeal stent effectiveness for OSA show mixed results, with some demonstrating significant improvement while others show limited benefit and tolerability. Some research suggests that nasal stents can reduce apnea events by 50% or more in a significant portion of patients. Other studies have shown less impressive results, with some finding stents no more effective than a placebo. Factors influencing effectiveness include the type of stent, OSA severity, individual anatomy, and proper stent placement. Ongoing research continues to explore long-term effectiveness and optimal patient selection. The 2015 publication by Cambridge University Press & Assessment acknowledges this variance in effectiveness and patient experience.
Patient Experience and Tolerability
Patient experience with nasopharyngeal stents varies, with some reporting improved sleep quality and reduced apnea episodes, while others experience discomfort or dislodgement. Some individuals may experience nasal congestion, dryness, or minor pain. Nosebleeds and stent dislodgement, while not common, are also potential risks. A proper fit is crucial for comfort and efficacy, highlighting the importance of working closely with a healthcare professional.
Benefits and Risks of Nasopharyngeal Stents
Potential Benefits:
- Minimally Invasive: Offers a less invasive alternative to surgery.
- CPAP Alternative: Provides an option for those who cannot tolerate CPAP.
- Snoring Reduction: May reduce or eliminate snoring.
- Improved Sleep Quality: Can potentially lead to more restful sleep.
Potential Risks:
- Discomfort: May cause nasal irritation, congestion, or dryness.
- Nosebleeds: A small risk of nosebleeds exists.
- Dislodgement: The stent may shift out of place.
- Infection: A slight risk of infection, as with any medical device.
How Long Do Nasal Stents Stay In?
The duration a nasal stent remains in place varies depending on the underlying condition, stent type, and individual healing. For minor procedures, it may be a few weeks, while more complex cases might require several months. Regular follow-up appointments are essential to monitor progress and determine the appropriate removal time. Adhering to post-stent care instructions, such as nasal irrigation and gentle cleaning, contributes to successful outcomes.
Conclusion
Nasopharyngeal stents can be a viable option for some individuals with OSA, especially those who haven’t found success with other treatments. However, it’s essential to have realistic expectations and understand that effectiveness and comfort vary from person to person. Consulting with a healthcare professional is crucial to determine if this treatment is appropriate for your specific situation. They can assess your condition, discuss potential benefits and risks, and guide you through the decision-making process. Ongoing research and technological advancements continue to shape our understanding of nasopharyngeal stents and their role in managing OSA.