Understanding Muscle Models in Healthcare
Muscle models are revolutionizing healthcare by providing dynamic, three-dimensional representations of the musculoskeletal system. These models transcend static images, enabling healthcare professionals and patients to explore the intricate mechanisms of muscles with unprecedented detail. This enhanced visualization facilitates improved understanding, diagnosis, and treatment of musculoskeletal conditions. For more information on advanced healthcare applications, check out this helpful resource.
Improved Patient Education: A patient facing rotator cuff surgery can better grasp the procedure through a muscle model demonstration. This visual aid transforms complex medical terminology into an easily understood format, empowering patients to actively participate in their care decisions. For instance, visualizing the affected tendons and the surgical repair process can alleviate patient anxiety and improve post-operative compliance with rehabilitation protocols.
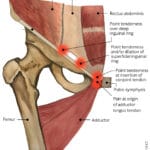
Enhanced Diagnostic Capabilities: Muscle models furnish healthcare professionals with a detailed “blueprint” of a patient’s musculoskeletal system. A physical therapist can precisely identify the specific muscles contributing to a patient’s back pain, guiding more targeted and effective treatment. This precision streamlines the diagnostic process, reducing the likelihood of misdiagnosis and accelerating the path to recovery. Consider a patient with chronic knee pain; a muscle model can pinpoint weaknesses in supporting muscles, informing tailored exercises to address the underlying cause.
Optimized Treatment Planning: Surgeons leverage muscle models to meticulously plan surgical approaches, visualize injuries, and even simulate procedures before entering the operating room. This pre-operative planning minimizes surgical risks and enhances precision. In joint replacement surgery, for example, surgeons can utilize models to optimize implant placement and alignment, potentially leading to reduced recovery times and improved long-term outcomes. Studies indicate that this pre-operative planning using 3D models can significantly decrease post-surgical complications and enhance patient satisfaction.
Refining 3D Muscle Models for Medical Education
Leveraging Technology for Enhanced Learning
3D muscle models provide medical students with a unique virtual exploration of the human body. Further refinement of these models through enhanced accuracy, accessibility, and curriculum integration unlocks their full educational potential.
Improving Accuracy and Detail: High-resolution CT and MRI scans form the basis for detailed 3D models. Incorporating realistic muscle fiber arrangements, anatomical variations, and interactive elements significantly deepens understanding of muscle function and contraction. For example, visualizing the sliding filament theory of muscle contraction in a 3D model can solidify this complex concept for students. This level of detail prepares students for the diversity of musculoskeletal presentations they will encounter in clinical practice.
Enhancing Accessibility and Usability: Intuitive software interfaces, open-source platforms, and mobile compatibility are essential for widespread adoption. Accessible tools allow students to explore anatomical structures at their own pace, reinforcing comprehension of complex concepts, anytime, anywhere. Interactive features, such as the ability to rotate, zoom, and isolate specific muscles, can enhance engagement and facilitate active learning.
Integrating Models into the Curriculum: Interactive learning modules, standardized protocols, and ongoing evaluation are crucial for effective pedagogical implementation. These models should become integral components of the medical curriculum, actively engaging students in their learning process. For instance, incorporating case studies where students utilize muscle models to diagnose and develop treatment plans can bridge the gap between theory and practice.
Muscle Models in Physical Therapy Rehabilitation
The Four-Element Model in Action
The four-element movement system model—motion, force, energy, and control—provides a robust framework for physical therapy practice. This model facilitates objective assessment, personalized goal setting, and targeted interventions, ultimately optimizing patient outcomes.
Assessment: The model guides therapists in systematically evaluating each element: motion (range of movement, joint mobility), force (muscle strength, power), energy (endurance, fatigue), and control (coordination, neuromuscular activation). This comprehensive approach ensures a thorough understanding of the patient’s specific movement dysfunction, such as identifying limited ankle dorsiflexion contributing to gait abnormalities.
Goal Setting: Based on the assessment, personalized treatment goals are established, targeting specific deficits within each element. For example, if a patient exhibits weakness in hip abductors, the goal might be to increase strength in these muscles to improve stability during walking. This focused approach maximizes the effectiveness of the therapeutic intervention.
Intervention: Tailored treatment programs are designed, incorporating exercises to improve strength, range of motion, coordination, and endurance, directly addressing the identified deficits. For instance, exercises with resistance bands targeting the hip abductors could be prescribed, with progress tracked and the program adjusted based on the patient’s response.
Personalizing Treatment with Muscle Models
The Power of Individualized Care
Personalized neuromusculoskeletal models empower clinicians to tailor mobility treatment to individual patient needs. This precision medicine approach requires precise data acquisition, model calibration, and user-friendly software, ultimately maximizing treatment effectiveness.
Building a Personalized Model: The process begins with comprehensive data acquisition via motion capture, strength assessments, and advanced imaging techniques like MRI and CT scans. These data inform the creation of a patient-specific digital twin of their musculoskeletal system. This model is meticulously calibrated to accurately reflect the patient’s unique anatomy, physiology, and movement patterns. For instance, a patient with scoliosis may have their model adjusted to reflect their spinal curvature, allowing for simulations of corrective exercises.
Designing Personalized Treatment: The calibrated model predicts the effects of various treatment options, enabling virtual experimentation with exercises, therapies, and even surgical interventions. This predictive capability optimizes treatment effectiveness and minimizes potential risks. For example, simulating the impact of different orthotics on a patient’s gait can help determine the most effective device.
Overcoming Challenges: Implementing personalized modeling entails challenges such as data acquisition costs, computational resources, and integration into existing clinical workflows. However, ongoing advancements in technology and research are actively addressing these challenges, paving the way for broader access to personalized neuromusculoskeletal care and ultimately improving patient outcomes.
- Georgia Platform: A Southern Strategy, 1850s - March 31, 2025
- How many weeks is 40 days: Quick Conversion Guide for Accurate Results - March 31, 2025
- How many feet is 300 meters? 984 Feet: Understand Length Conversions Easily - March 31, 2025