Embark on “A Journey Through Time: The Evolution of Medical Records Management,” where we delve into the captivating history of a field dedicated to preserving the integrity of patient information. From ancient papyrus scrolls to modern electronic health records, witness the remarkable transformation of medical record-keeping practices and the pivotal role they have played in shaping healthcare’s evolution.
Key Takeaways:
- Medical records have a rich history, originating in ancient times.
- They initially served an educational purpose, but later became essential for insurance, legal matters, and patient care.
- The US medical record reached its modern form in 1898, featuring comprehensive bedside notes.
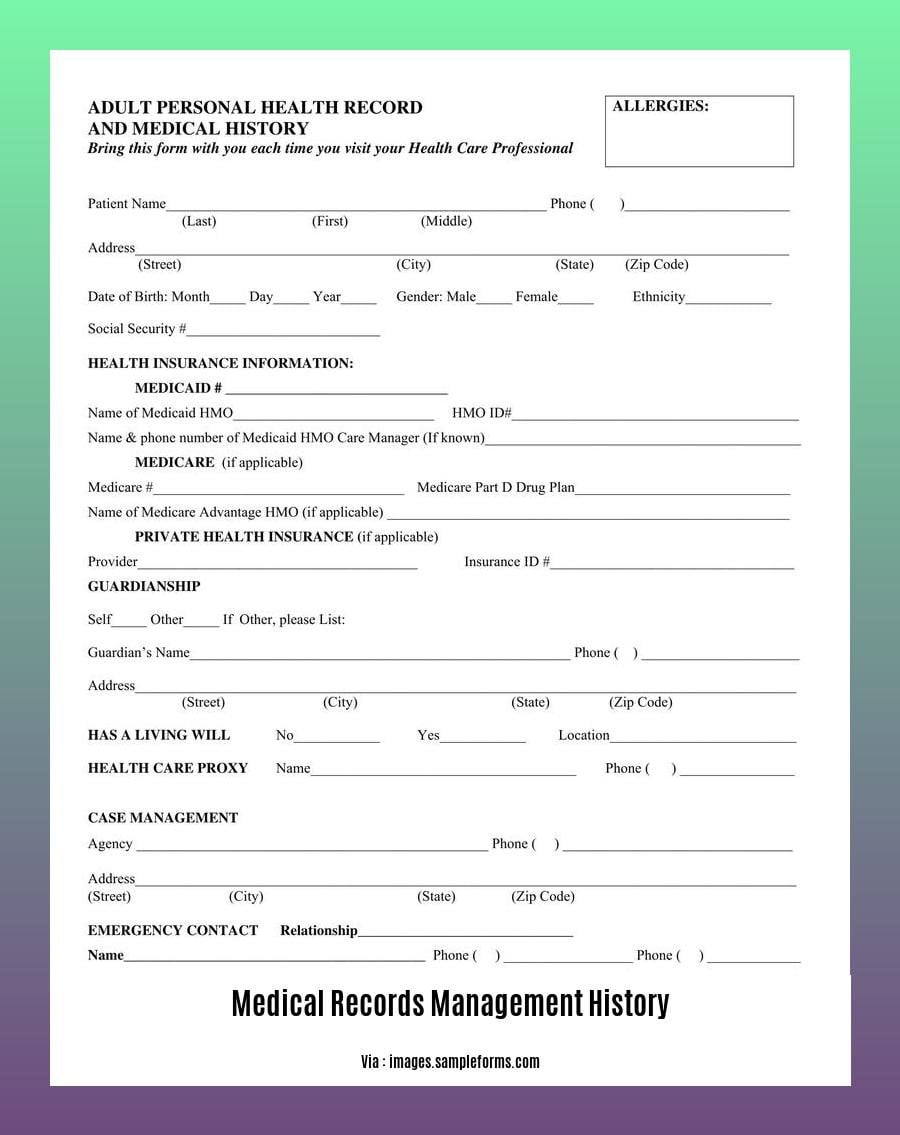
Medical Records Management History
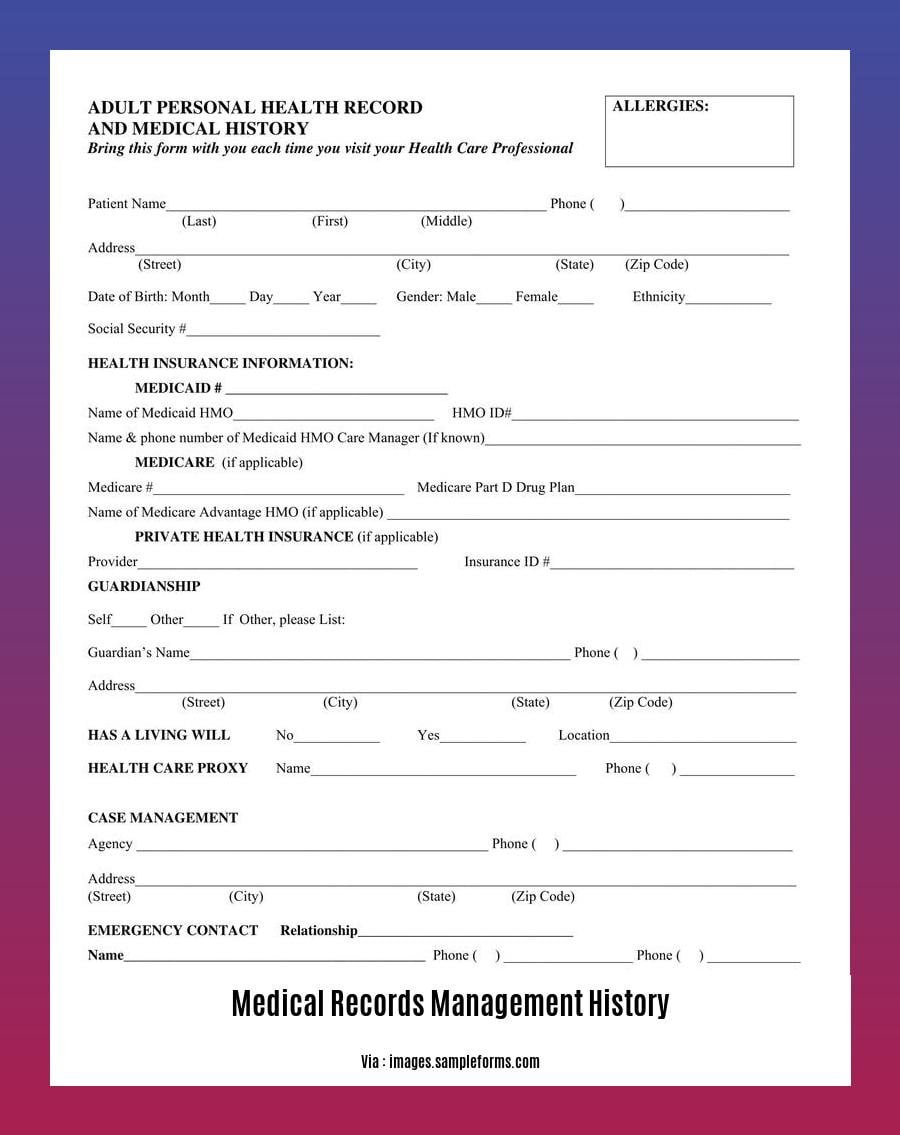
Our medical records hold a fascinating history. Their journey began in ancient times, serving as educational tools for aspiring physicians. Over centuries, they evolved into indispensable instruments for insurance, legal matters, and the cornerstone of patient care.
Ancient Roots:
In the bustling streets of ancient Greece, medical records were inscribed on clay tablets, capturing patients’ symptoms and treatments. These rudimentary records laid the foundation for future medical advancements.
Middle Ages Musings:
Fast forward to medieval Europe, where medical records took a more literary turn. Physicians filled pages with detailed patient accounts, often accompanied by vivid illustrations. These records served as case studies, providing invaluable insights into the diseases of the time.
19th Century Revolution:
A watershed moment occurred in 1898 when medical records management history reached a turning point. American physicians began recording detailed bedside notes, transforming medical records into the comprehensive accounts we recognize today.
20th Century Advancements:
The 20th century ushered in a whirlwind of technological advancements. Medical records migrated from paper to digital formats, allowing for easier storage, retrieval, and sharing of patient information.
Modern Era:
Today, medical records management history continues to evolve at a rapid pace. Electronic health records (EHRs) seamlessly integrate patient data across various healthcare providers, enhancing care coordination and decision-making. Artificial intelligence and machine learning are also revolutionizing the field, promising to improve accuracy, efficiency, and patient outcomes.
As we embark on this medical records management history journey, remember that these records are not mere pieces of paper or digital files. They embody the rich tapestry of healthcare, preserving the stories of our ancestors and shaping the future of medicine.
Did you know the history of health information management dates back to ancient civilizations? Over time, health information management has evolved dramatically, and so has its impact on healthcare. Learn about the rich HIM history that has shaped the field into what it is today.
Computerization and Digitization: Transforming Medical Records Management
The shift towards the computerization and digitization of medical records has revolutionized the way we store, retrieve, and manage patient information. This digital transformation has brought about significant benefits, including:
Increased efficiency: Digital records streamline workflows, eliminate manual processes, and reduce the storage space required for physical records.
Reduced errors: Digital systems can perform quality checks and reduce the risk of transcription errors, ensuring the accuracy of patient information.
Improved patient care: Computerization and digitization enhance accessibility and integration of patient data, enabling healthcare professionals to make informed decisions and provide better care.
Key Takeaways:
- Digitalisation has enhanced storage, retrieval and sharing of patient data
- A computerised system can perform quality checks and prevent transcription errors
- Computerization and digitization improve the accessibility and integration of patient data
Relevant URL Source:
- A History of the Shift Towards Full Computerization of Medicine by Edward P. Ambinder
Legal and Ethical Issues
As medical records transition into the digital realm, they bring forth a myriad of legal and ethical challenges. Let’s delve into these sensitive issues and explore their implications for patient care:
Confidentiality and Privacy
Electronic medical records (EMRs) contain vast amounts of sensitive patient data, making confidentiality and privacy paramount concerns. Unauthorized access or misuse of this information can have severe consequences, necessitating robust safeguards to protect patient privacy.
Patient Autonomy and Consent
EMRs raise questions about patient autonomy and informed consent. Patients should have control over their health information, including the right to decide who can access it. Ensuring that patients fully understand and consent to the sharing of their medical data is crucial for respecting their autonomy.
Beneficence and Non-Maleficence
The principle of beneficence requires healthcare professionals to act in the best interests of their patients. EMRs can enhance patient care through improved data sharing and decision-making, but it’s essential to balance these benefits against potential risks. Non-maleficence ensures that EMRs are not used in ways that harm patients.
Fidelity and Honesty
Medical records must be accurate and truthful, reflecting the patient’s health status. EMRs have the potential to facilitate deception or fraud, making it imperative to establish clear guidelines and mechanisms for ensuring the fidelity of the data they contain.
Cost-Effectiveness
EMRs represent a significant investment for healthcare organizations. Ensuring their cost-effectiveness is crucial. Balancing the upfront costs of implementation and maintenance with the long-term benefits for patient care and organizational efficiency is essential.
Key Takeaways:
- Confidentiality and privacy concerns arise with the vast amount of patient data stored in EMRs.
- Patient autonomy and informed consent are crucial for ensuring patient control over their health information.
- Beneficence and non-maleficence require balancing the benefits of EMRs with potential risks to patients.
- Fidelity and honesty are essential for maintaining the accuracy and truthful nature of medical records.
- Cost-effectiveness is a key consideration in evaluating the implementation and maintenance of EMRs.
Citation:
- Ethical Issues in Electronic Health Records: A General Overview. (2015). National Library of Medicine.
Future Trends
Technology continues to sculpt the landscape of medical records management. The evolution of Future Trends promises to transform healthcare delivery, offering unprecedented opportunities for improving patient care and efficiency.
Key Takeaways:
Enhanced Interoperability: Future Trends aims to break down silos and promote seamless data exchange across healthcare systems. Patients will benefit from a comprehensive view of their medical history, empowering them with better-informed decisions.
Patient Empowerment: Future Trends recognizes the patient as the central figure in healthcare. Patient portals and other self-service tools will grant patients greater access to their records and enable them to actively participate in their care plans.
Predictive Analytics: Future Trends harnesses the power of data to predict patient outcomes. By analyzing vast amounts of medical information, healthcare providers can identify high-risk patients, optimize treatment protocols, and prevent adverse events.
Artificial Intelligence (AI) and Machine Learning (ML): Future Trends integrates AI and ML to automate tasks, improve accuracy, and enhance decision-making. These technologies assist in medical image analysis, natural language processing, and fraud detection, reducing human error and streamlining workflows.
Important URL Sources:
FAQ
Q1: When did medical records first come into use?
A1: Medical records have a long history dating back to ancient civilizations. They were initially used for educational purposes but evolved into a vital tool for insurance, legal procedures, and patient care. By 1898, US medical records became complete in today’s sense, including detailed notes at the bedside.
Q2: How did the widespread use of electronic medical records (EMRs) come about?
A2: The shift towards full computerization of medicine began in 1991 when the Institute of Medicine (IOM) recognized the potential of EMRs. In 2004, President George W. Bush called for computerized health records in his State of the Union Address. The American Recovery and Reinvestment Act (ARRA) in 2009 accelerated the adoption of EHRs, and their digitization continues to enhance efficiency, reduce errors, and improve patient care.
Q3: What are some ethical concerns related to EMRs?
A3: EMRs raise ethical concerns regarding patient privacy and security, autonomy, beneficence, non-maleficence, fidelity and honesty, and cost-effectiveness. Privacy concerns arise due to the vast amount of sensitive patient data stored in EMRs, and the potential for unauthorized access or misuse. Autonomy concerns relate to the patient’s right to make informed decisions about their own health care, and the potential for EMRs to limit patient choice or control over their data.
Q4: How have EHRs evolved over time?
A4: EHRs were in their early stages of development in 1992, with limited functionality and interoperability. By 2015, they had become widely adopted and offered advanced features such as patient portals and decision-support tools. Future expectations for EHRs include improved interoperability, patient engagement, and predictive analytics. The evolution of EHRs has been accelerated by technological advancements and government incentives.
Q5: How should HIM professionals adapt to the changing landscape of health data management?
A5: HIM professionals need to adapt to the changing landscape of health data management by embracing new technologies and evolving their skills. This includes becoming proficient in data analytics, information governance, and cybersecurity. They should also stay updated on regulatory changes and best practices in the field.
- China II Review: Delicious Food & Speedy Service - April 17, 2025
- Understand Virginia’s Flag: History & Debate - April 17, 2025
- Explore Long Island’s Map: Unique Regions & Insights - April 17, 2025