This guide provides healthcare professionals and new parents with a comprehensive understanding of fundal massage, its purpose, technique, benefits, and potential considerations.
Understanding Fundal Massage
After childbirth, the uterus, which has expanded significantly during pregnancy, needs to return to its pre-pregnancy size. This process, called involution, is aided by fundal massage. The fundus is the top portion of the uterus, and massaging it helps to stimulate contractions, reduce bleeding, and promote healing.
What is the Fundus?
The fundus is the topmost part of the uterus. After delivery, it feels like a firm, grapefruit-sized mass just below the belly button. Locating and massaging this area is key to promoting postpartum recovery. For a deeper understanding of the anatomy and physiology involved, you might find our morphine sulfate medication template helpful in understanding how medications can interact with this process.
Why Massage the Fundus?
Fundal massage serves several crucial purposes:
- Preventing Postpartum Hemorrhage (PPH): PPH, or excessive bleeding after delivery, is a serious complication. Fundal massage stimulates uterine contractions, helping to constrict blood vessels and minimize bleeding. This proactive approach reduces the likelihood of needing more invasive interventions. A “boggy uterus,” characterized by softness and poor contraction, is a strong indicator for fundal massage.
- Aiding Uterine Involution: Massaging the fundus encourages the uterus to contract and shrink back to its pre-pregnancy size. This process is essential for long-term uterine health.
- Reducing Pain and Discomfort: While the massage itself can be momentarily uncomfortable, it ultimately helps to reduce postpartum cramping and pain. The contractions stimulated by the massage can feel like strong menstrual cramps, or a forced contraction, but this discomfort is generally temporary. The perceived intensity varies widely among individuals.
- Minimizing Medication Needs: In some cases, fundal massage can lessen the need for uterotonic medications, which are drugs used to induce uterine contractions.
Performing Fundal Massage
Technique
Proper technique is essential for effective and safe fundal massage:
- Locate the fundus: Gently palpate the abdomen to locate the top of the uterus. It will feel like a firm mass, usually a few inches below the belly button.
- Support the lower uterus: Place one hand just above the pubic bone to support the lower part of the uterus. This stabilizes the uterus and prevents undue strain during the massage. This support is vital in preventing uterine inversion, a rare but serious complication.
- Massage the fundus: Using a circular motion, apply firm but gentle pressure to the fundus. Avoid vigorous rubbing, as this can cause unnecessary pain and bruising.
- Assess uterine tone: Throughout the massage, assess the firmness of the uterus. A firm uterus indicates effective contractions. A soft, or “boggy,” uterus suggests the need for continued massage.
- Monitor bleeding: Observe the amount of bleeding before, during, and after the massage. A decrease in bleeding suggests the massage is effective.
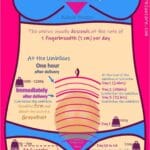
Timing and Frequency
The timing and frequency of fundal massage are crucial aspects of postpartum care. Typically, the massage begins shortly after placental delivery:
- First Hour: Every 10-15 minutes. This frequent assessment is critical in the immediate postpartum period when the risk of hemorrhage is highest.
- Second Hour: Every 30 minutes. As the uterus begins to firm up, the frequency may decrease.
- Subsequent Hours: Varies by hospital protocol and individual needs. Some hospitals may continue checks every 30-60 minutes, while others might reduce it to hourly or less frequent checks. While there are established initial guidelines, standardized protocols for subsequent hours are lacking, emphasizing the need for individualized assessment and clinical judgment. Ongoing research aims to determine the most effective and comfortable long-term frequency.
Fundal Assessment vs. Fundal Massage
It’s important to distinguish between fundal assessment and fundal massage. Assessment involves gentle palpation to determine the location, firmness, and height of the fundus. Massage, on the other hand, is an active intervention designed to stimulate contractions. As Barbie Christia notes, “So again, the massage is also being assessed, but it is not a fundal assessment. It is an actual intervention.“
The Patient Experience
Fundal massage can be uncomfortable, sometimes causing sensations similar to strong menstrual cramps or a forced contraction. Open communication with the patient is essential. Explain the purpose and importance of the procedure, reassuring them that the discomfort is temporary and necessary for their recovery.
Managing Discomfort
Several strategies can help minimize discomfort:
- Deep breathing and relaxation techniques: Encourage the patient to practice deep, slow breaths to relax their abdominal muscles.
- Warm compresses: Applying a warm compress to the lower abdomen may help soothe the muscles and ease cramping.
- Skin-to-skin contact: Studies suggest that skin-to-skin contact with the baby may reduce perceived discomfort during fundal massage, highlighting the interconnectedness of physical and emotional well-being in postpartum care.
- Pain medication: If needed, over-the-counter pain relievers, such as ibuprofen or acetaminophen, can be offered. However, always consult with the healthcare provider before administering any medication, especially if the patient is breastfeeding. If you’re exploring non-invasive comfort measures, our microderm infusion therapy might be of interest in a different context of care.
Ongoing Research and Future Directions
While fundal massage is a well-established practice, research is ongoing. Some areas of active study include:
- Standardized protocols: Developing evidence-based guidelines for the optimal frequency and duration of fundal massage beyond the initial postpartum hours.
- Alternative and complementary therapies: Exploring the effectiveness of complementary approaches, like aromatherapy or relaxation techniques, to enhance patient comfort during the procedure.
- Long-term effects: Investigating the potential long-term benefits of fundal massage on uterine health and future pregnancies.
Conclusion
Fundal massage is a vital component of postpartum care. While sometimes uncomfortable, this brief procedure plays a critical role in preventing postpartum hemorrhage, promoting uterine involution, and minimizing the need for more invasive interventions. By utilizing proper technique, open communication, and ongoing assessment, healthcare providers can ensure the safe and effective delivery of this essential care.