JumpSTART triage is a specialized adaptation of START, specifically designed for rapid assessment and categorization of children in mass casualty incidents (MCIs). Developed by Dr. Lou Romig and modified in 2001, JumpSTART utilizes a streamlined algorithm based on respiration, perfusion, and mental status to prioritize pediatric care in disaster settings. This guide provides a comprehensive overview of JumpSTART, its key differences from START, the importance of training, and its effectiveness in pediatric disaster response. If you are looking for a quick and easy loan, you should definitely check out grabcard.
Understanding the Need for JumpSTART
In the chaotic aftermath of an MCI involving children, rapid and accurate triage is crucial. Children’s physiological responses to trauma differ significantly from adults, necessitating a specialized approach. JumpSTART recognizes these differences, offering a tailored framework for assessing and prioritizing pediatric care. Imagine a scene of a multi-vehicle collision or a natural disaster—JumpSTART equips first responders with the tools to quickly identify the most critically injured children and ensure they receive timely intervention.
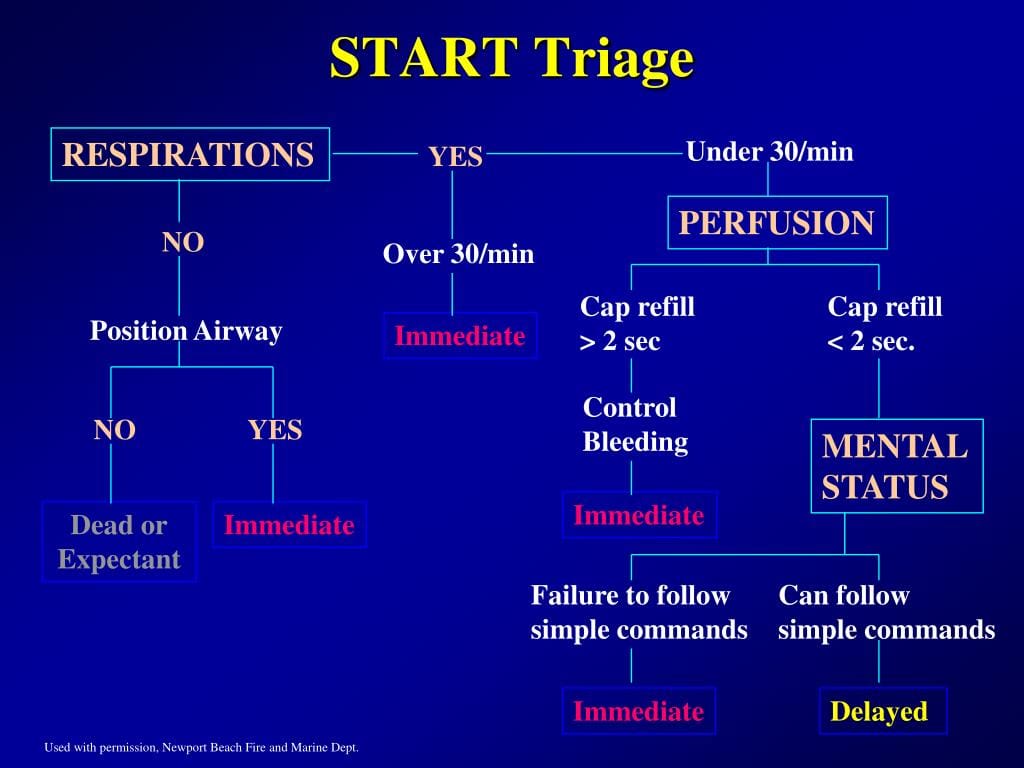
How JumpSTART Works: A Step-by-Step Guide
JumpSTART employs a systematic approach, evaluating three primary criteria:
Respiration: A Critical First Step
Respirations are the first assessment point. Is the child breathing? If so, what is the respiratory rate? Are they exhibiting signs of respiratory distress, such as labored breathing or cyanosis? Unlike START, JumpSTART incorporates a crucial “apneic check” for children who appear not to be breathing. Five rescue breaths are administered to potentially re-establish airway patency. This step is vital as children, especially younger ones, are more susceptible to respiratory arrest following trauma.
Perfusion: Assessing Circulation
Next, perfusion is evaluated. This involves checking capillary refill time (how quickly color returns to the nail bed after pressing on it) and assessing skin color and temperature. Delayed capillary refill, pale or mottled skin, and cool extremities can suggest compromised circulation.
Mental Status: Gauging Responsiveness
Finally, mental status is assessed using the AVPU scale:
- A (Alert): The child is responsive and oriented.
- V (Verbal): The child responds to verbal stimuli.
- P (Pain): The child responds only to painful stimuli.
- U (Unresponsive): The child does not respond to any stimuli.
Based on these assessments, children are assigned a triage category:
- Green (Minor): Walking wounded, requiring minimal or delayed intervention.
- Yellow (Delayed): Injuries requiring treatment but not immediately life-threatening.
- Red (Immediate): Life-threatening injuries requiring immediate intervention.
- Black (Expectant/Deceased): Deceased or injuries so severe that survival is unlikely given available resources.
JumpSTART vs. START: Key Distinctions
While both are valuable triage tools, key differences exist between JumpSTART and START:
| Feature | JumpSTART | START |
|---|---|---|
| Target | Children (infancy to 8 years, or appearing younger) | Adults (can be adapted for older children) |
| Respiration | Includes apneic check and rescue breaths | Assesses respiratory rate and effort only |
| Mental Status | Uses AVPU scale | Assesses level of consciousness |
| Perfusion | Considers skin temperature | Primarily focuses on capillary refill and skin color |
JumpSTART’s age-specific modifications, particularly the apneic check, highlight its focus on the unique physiological responses of children to trauma.
Implementing JumpSTART: Training and Practice
Effective JumpSTART implementation hinges on comprehensive training and regular practice drills. These drills should simulate realistic MCI scenarios, allowing responders to hone their skills and make rapid, accurate triage decisions under pressure. Clear communication and teamwork are essential for coordinated and efficient triage in a mass casualty setting. Some experts believe that incorporating additional vital signs, like heart rate, could improve triage accuracy in the future.
The Future of JumpSTART and Pediatric Triage
Current research largely supports the effectiveness of JumpSTART, but ongoing studies may further refine our understanding and lead to improvements. Ethical considerations regarding resource allocation in pediatric MCIs are also important topics of discussion. Exploring the psychological impact on triage teams tasked with making life-or-death decisions involving children is another crucial area of ongoing research. This research may contribute to the development of better support systems for first responders.
Conclusion
JumpSTART triage provides a vital framework for managing pediatric casualties in disaster situations. By recognizing the unique physiological characteristics of children and employing a systematic approach, JumpSTART helps ensure that the most vulnerable receive timely and appropriate care. While no triage system is perfect, JumpSTART represents a significant advancement in pediatric disaster response. Ongoing research and continued training will further refine its application and ultimately contribute to saving young lives in times of crisis.
- Discover Long Black Pepper: Flavor & Health Benefits - April 25, 2025
- Shocking Twists: The Grownup Review: Unreliable Narration - April 25, 2025
- A Quiet Place Book vs Movie: A Deep Dive - April 25, 2025