This article explores the troubling practice of involuntary seclusion in nursing homes, examining its definition, impact, and potential solutions. We’ll differentiate it from medically necessary isolation, discuss warning signs, and emphasize the importance of advocating for resident rights and dignity.
What is Involuntary Seclusion?
Involuntary seclusion is the confinement of a nursing home resident to a room or area against their will, without a valid medical or safety reason. It differs significantly from medically necessary isolation, a temporary measure implemented for the safety of the resident or others, such as during a contagious illness. While isolation is explained clearly to the resident and family, involuntary seclusion is often used for staff convenience or to control “difficult” residents. Discover how integral of x secx is calculated in mathematics.
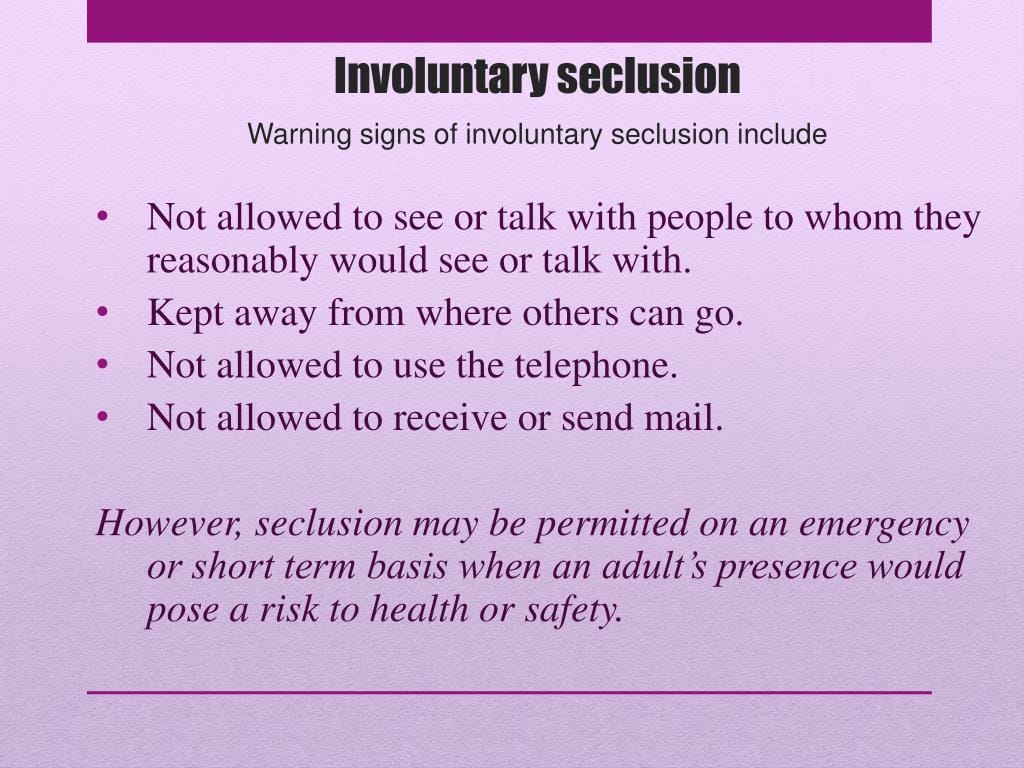
Recognizing the Warning Signs
Several red flags may suggest involuntary seclusion. Is the resident consistently confined without a clear explanation? Are they prevented from social activities or visits? Are physical restraints used without consent or for seemingly unreasonable causes? Do staff members avoid questions or provide vague answers about the resident’s whereabouts? These signs warrant further investigation.
The Devastating Impact of Involuntary Seclusion
The psychological consequences of involuntary seclusion can be severe. Imagine the feeling of being trapped, powerless, and forgotten. This can lead to increased anxiety, depression, and even post-traumatic stress disorder. Some experts believe the trauma is comparable to that experienced by prisoners of war or kidnapping victims, suggesting the need for specialized therapy. Delve into its techniques, benefits, and practical implementation for empowering communication skills. Involuntary seclusion may also worsen existing health conditions and potentially contribute to premature death. Residents may withdraw socially, exhibit increased aggression, or experience a significant decline in overall well-being.
Prevention and Intervention
Combating involuntary seclusion requires vigilance and action. If you suspect a resident is being secluded, report your concerns to the nursing home administration, the resident’s doctor, the local ombudsman, or state and federal agencies. Prevention efforts include advocating for better staff training on managing challenging behaviors respectfully, increased monitoring of residents by staff and family, and stronger regulations and oversight of nursing homes.
Real-World Examples of Involuntary Seclusion
Involuntary seclusion can manifest in various subtle ways. A resident might be consistently sent to their room after dinner against their wishes, prevented from participating in social activities without a valid reason, or subtly confined through unnecessary physical restraints. While bed rails might be presented as a safety measure, they can become a means of seclusion if the resident is capable of moving independently.
Distinguishing Involuntary Seclusion from Medically Necessary Isolation
The crucial difference lies in the purpose and justification. Involuntary seclusion is often punitive or for staff convenience, imposed against the resident’s will, and can be prolonged indefinitely without a valid reason. Medically necessary isolation, conversely, aims to protect the resident or others from health risks, is usually short-term and justified by a physician, and even when against a resident’s wishes, is reasonable and explained as so.
Understanding Voluntary Seclusion
Voluntary seclusion, unlike its involuntary counterpart, is self-imposed isolation chosen by the individual. This could be for various reasons, such as needing a break from social interaction, focusing on a project, or engaging in self-reflection.
Voluntary Seclusion in Healthcare
In healthcare settings, respecting patient autonomy while ensuring their well-being presents a complex challenge. Healthcare professionals must determine if the seclusion is truly voluntary and not driven by underlying mental health conditions like depression or social anxiety. Ongoing research explores the nuances of voluntary seclusion and its varying effects on individuals.
Examples of Seclusion
While we’ve discussed specific examples within nursing homes, it’s important to understand that seclusion can occur in other settings. In schools, isolating a student in a “time-out” room for excessive periods without justification is a likely form of involuntary seclusion if the student poses no immediate threat. In hospitals, using restraints on a non-threatening patient can also be considered a form of seclusion. Some experts suggest the overuse of restraints, even without a locked room, constitutes seclusion if it severely limits movement, though ongoing research continues to explore the nuances of this issue. Other examples of involuntary seclusion may appear more like a form of “house arrest”. This could include restricting the resident’s movements within the facility itself, even if they are not confined to a single room.
Recognizing Potential Signs
While the following are not definitive proof, they are warning signs that may suggest seclusion: restricted movement without a clear reason, isolation from loved ones, and changes in behavior such as increased anxiety, withdrawal, or aggression.
Conclusion
Understanding the difference between voluntary and involuntary seclusion, recognizing the warning signs, and acting on concerns are vital steps in protecting vulnerable individuals. By working together, we can promote a more humane and respectful environment in nursing homes and other settings. While research continues to evolve our understanding of seclusion, the potential for harm underscores the need for vigilance and advocacy.
- Unlock Water’s Symbolism: A Cross-Cultural Exploration - April 20, 2025
- Identify Black and White Snakes: Venomous or Harmless? - April 20, 2025
- Unlocking Potential: Origins High School’s NYC Story - April 20, 2025










2 thoughts on “Combating Involuntary Seclusion in Nursing Homes: Protecting Rights & Preserving Dignity”
Comments are closed.