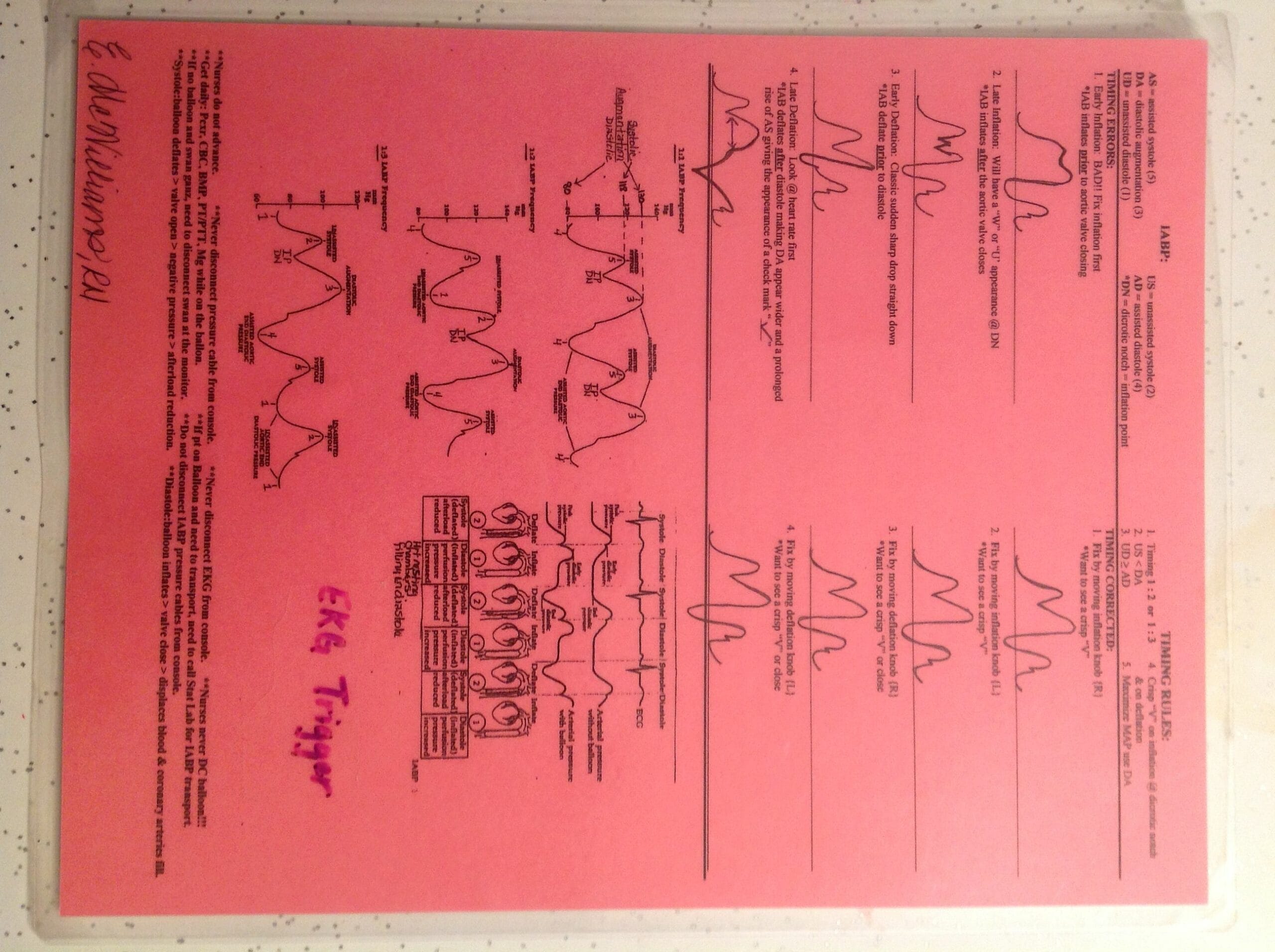
This guide provides a comprehensive overview of intra-aortic balloon pump (IABP) waveforms, focusing on interpretation and troubleshooting. Understanding these waveforms is crucial for optimizing IABP therapy and improving patient outcomes.
Decoding the IABP Waveform
The IABP waveform is a visual representation of pressure changes within the aorta and the IABP balloon itself. It provides real-time insights into the interaction between the heart and the IABP. By learning to interpret this waveform, clinicians can fine-tune IABP timing, maximize its effectiveness, and promptly identify potential issues.
Key Components of the IABP Waveform
The IABP waveform has several key features:
- Unassisted Systolic Pressure: The peak pressure the heart generates independently, without IABP assistance.
- Assisted Aortic End-Diastolic Pressure: The lowest aortic pressure just before the next heartbeat. The IABP helps increase this pressure, benefiting coronary artery perfusion.
- Augmented Diastolic Pressure: The increased pressure resulting from IABP inflation. This boosts systemic and coronary blood flow.
- Dicrotic Notch: A small dip in the waveform indicating aortic valve closure. This is a critical landmark for IABP timing.
Mastering IABP Timing
Precise timing of IABP inflation and deflation is essential for optimal support. Ideally, inflation occurs just before the dicrotic notch (approximately 40 milliseconds earlier), while deflation occurs just before the next heartbeat, signaled by the R-wave on the ECG. Incorrect timing can reduce IABP effectiveness and may even lead to complications.
Troubleshooting IABP Waveform Abnormalities
Recognizing and addressing abnormal waveforms is crucial. Here are some common issues:
- Early Inflation: Inflation before the dicrotic notch may blunt augmented diastolic pressure. This can be corrected by adjusting the IABP trigger to delay inflation.
- Late Deflation: Deflation after the R-wave can elevate unassisted systolic pressure and hinder ventricular filling. Adjusting the IABP trigger for earlier deflation usually resolves this.
- Inadequate Augmentation: A small increase in diastolic pressure suggests suboptimal IABP support. This may be due to incorrect balloon position, catheter leaks, insufficient gas in the balloon, or other factors requiring investigation.
The Normal IABP Waveform: A Rhythmic Dance
The normal IABP waveform reflects a synchronized interaction between the heart and the IABP. It shows a characteristic pattern of pressure changes: a sharp rise during inflation, a sustained elevated pressure during diastole, and a rapid drop during deflation. This optimized counterpulsation enhances coronary and systemic perfusion. The dicrotic notch and R-wave serve as crucial timing landmarks for inflation and deflation, respectively, maximizing hemodynamic benefit and minimizing left ventricular workload. The augmented diastolic pressure should create a distinct, sharp V shape on the arterial waveform, exceeding the previous systolic peak. This sharp V-shaped augmented diastolic pressure is a hallmark of effective IABP support. However, it’s important to note that variations can occur depending on individual patient factors and underlying conditions. Ongoing research continues to explore the nuances of these interactions, and some experts believe subtle waveform differences may provide further insights into cardiac function. For more information on the brain’s memory function, you can delve into the intricacies of the hippocampus.
| Feature | Description | Timing |
|---|---|---|
| Inflation | Sharp pressure rise, balloon inflates | Just before the dicrotic notch |
| Augmented Diastolic Pressure | Higher-than-normal diastolic pressure | During diastole, after balloon inflation |
| Deflation | Sharp pressure drop, balloon deflates | Just before the R wave on the EKG |
Late IABP Inflation: Recognizing the “W” Waveform
Late IABP inflation, occurring after the dicrotic notch, disrupts the normal waveform and diminishes the pump’s effectiveness. This delay reduces diastolic augmentation, potentially compromising coronary perfusion and increasing afterload. Visually, it creates a characteristic “W” shape on the arterial pressure tracing. This altered morphology signals a need for prompt intervention to optimize hemodynamic support. Troubleshooting involves verifying trigger timing, catheter position, and addressing patient-specific factors to restore effective counterpulsation. While research has illuminated much about this phenomenon, ongoing studies continue to refine our understanding and treatment strategies.
| Feature | Normal IABP Inflation | Late IABP Inflation |
|---|---|---|
| Inflation Timing | Early diastole | After dicrotic notch |
| Waveform Shape | Smooth curve | “W” shape |
| Effects | Increased diastolic pressure, decreased systolic pressure, improved coronary perfusion | Reduced diastolic augmentation, potentially compromised coronary perfusion |
How the IABP Works: The Principle of Counterpulsation
The IABP utilizes the principle of counterpulsation to support the failing heart. It strategically augments coronary blood flow and reduces cardiac workload through precisely timed balloon inflation and deflation within the aorta, synchronized with the cardiac cycle. During diastole, inflation increases diastolic aortic pressure, improving coronary artery perfusion and enhancing systemic perfusion. Conversely, during systole, deflation decreases systolic aortic pressure (afterload), reducing left ventricular workload and myocardial oxygen demand. Precise IABP timing, typically triggered by the ECG’s R-wave, is crucial for optimal hemodynamic support. The effectiveness of IABP therapy is evaluated by observing changes in aortic pressure characteristics, including augmented diastolic pressure, reduced systolic pressure, and increased mean arterial pressure. While the IABP console provides the most accurate mean arterial pressure measurement, central aortic pressure monitoring via the IABP lumen is considered the gold standard. This understanding is critical for clinicians making decisions about patient care. You can find information on energy efficiency standards in IECC 2018.
| IABP Phase | Heart Cycle Phase | Balloon Status | Effect |
|---|---|---|---|
| Inflation | Diastole | Inflated | Increased coronary & diastolic pressure |
| Deflation | Systole | Deflated | Decreased afterload, reduced cardiac work |
Conclusion: The Power of Waveform Interpretation
Mastering IABP waveform interpretation empowers clinicians to optimize IABP therapy, enhancing its effectiveness and improving patient outcomes. By recognizing both normal and abnormal waveform patterns, healthcare professionals can quickly identify and address potential complications, ensuring the best possible support for patients with compromised cardiac function. While our understanding of IABP therapy continues to evolve through ongoing research, the ability to interpret the IABP waveform remains a cornerstone of effective clinical management. This ongoing research may lead to further advancements in IABP technology and further refine our understanding of optimal IABP implementation.
- Unlock Elemental 2 Secrets: Actionable Insights Now - April 2, 2025
- Lot’s Wife’s Name: Unveiling the Mystery of Sodom’s Fall - April 2, 2025
- Photocell Sensors: A Complete Guide for Selection and Implementation - April 2, 2025