Journey through the fascinating history of Emergency Medical Services (EMS) in our in-depth article, [[History of EMS Timeline]: A Journey from Humble Beginnings to Sophisticated Healthcare]. Dive into the evolution of EMS from its modest origins to the highly regulated, advanced system we rely on today. Discover the pivotal moments, innovations, and challenges that have shaped this critical field of healthcare.
Key Takeaways:
Dr. Jonathan Letterman established the Ambulance Corps, emphasizing organized medical care during the Civil War (1865).
Pre-hospital emergency care lacked trained personnel, adequate equipment, and standardized response times before the 1960s.
Dr. Peter Safar revolutionized CPR techniques with his work, “ABCs of Resuscitation” (1966).
The National Academy of Sciences’ White Paper highlighted the need for a comprehensive EMS system in 1967.
Paramedic training programs emerged in the 1970s, offering advanced medical training to pre-hospital personnel.
The NREMT was established to ensure standardized training and competence for EMTs (1970s).
The first 911 emergency telephone number was implemented in the US in 1973, providing a centralized system for emergencies.
The Emergency Medical Services Systems Act, passed in 1974, provided federal support for EMS system development.
Advanced medical equipment and technology, like defibrillators, became more widespread in EMS during the 1980s.
The 1990s saw a focus on improving patient care through evidence-based practices and continuous education for EMS providers.
History of EMS Timeline
Throughout the annals of healthcare, the evolution of Emergency Medical Services (EMS) stands as a testament to the remarkable strides made in providing timely and effective medical care to those in need. Delve into the history of EMS timeline, tracing its humble origins to the sophisticated, highly regulated system we know today.
Pre-1960s: A Patchwork of Care
Before the 1960s, emergency medical care was a fragmented landscape, characterized by poorly trained personnel, rudimentary equipment, and inconsistent response times. This era saw the rise of volunteer ambulance services, primarily staffed by individuals with minimal medical training.
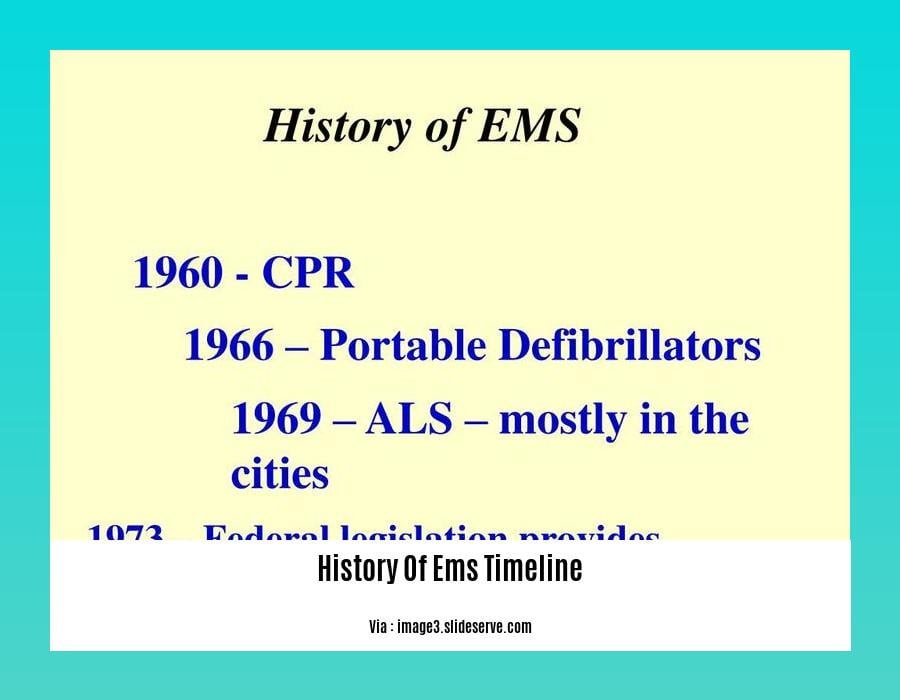
1960s: The Seeds of Transformation
The 1960s ushered in a period of profound change for EMS. Dr. Peter Safar’s groundbreaking work on cardiopulmonary resuscitation (CPR) techniques revolutionized emergency care, while the National Academy of Sciences’ White Paper on Accidental Death and Disability highlighted the urgent need for a comprehensive EMS system.
1970s: The Dawn of Paramedics
The 1970s marked a pivotal era with the emergence of paramedic training programs, offering advanced medical training to pre-hospital personnel. This decade also witnessed the establishment of the National Registry of EMTs (NREMT), ensuring standardized training and competence for emergency medical technicians (EMTs).
1973: The Advent of 911
The implementation of the 911 emergency telephone number in 1973 provided a centralized system for reporting emergencies, streamlining access to medical care.
1974: Federal Recognition and Support
In 1974, the United States Congress passed the Emergency Medical Services Systems Act, demonstrating the federal government’s commitment to developing a nationwide EMS system. This act provided funding and support for the establishment of standardized protocols, training, and coordination among emergency responders.
1980s: Technological Advancements
The 1980s saw the widespread adoption of advanced medical equipment and technology in EMS, including defibrillators and advanced airway management devices. These advancements significantly improved the quality of care provided to patients in emergency situations.
1990s and Beyond: Continuous Improvement
The 1990s ushered in an era of continuous improvement in EMS, with a focus on evidence-based practices, quality improvement initiatives, and ongoing education for EMS providers. This period also saw the rise of specialized EMS teams, such as hazardous materials response units and tactical medical teams.
Today, EMS stands as a cornerstone of modern healthcare, providing critical care to patients in their time of need. The history of EMS timeline serves as a reminder of the dedication, innovation, and collaboration that have shaped this essential service.
Discover the fascinating history of the digital printing industry and its captivating journey from traditional methods to cutting-edge technologies in our in-depth article on the history of digital printing.
Embark on a journey through the history of disc golf, a sport that combines the thrill of competition, precision, and the serene beauty of nature. Learn about its captivating evolution from humble beginnings to becoming a globally recognized sport in our comprehensive article on the history of disc golf.
Explore the rich heritage of dressmaking, an art form that has adorned cultures worldwide for centuries. Uncover the intricate techniques, styles, and cultural influences that have shaped this creative field in our captivating piece on the history of dressmaking.
Delve into the world of English drama of the 11th class, a period marked by literary genius, cultural shifts, and theatrical innovations. Discover the captivating stories, themes, and playwrights that defined this era in our comprehensive exploration of the history of English drama 11th class.
Standardization and Regulation: The Rise of Professional Standards in EMS
The evolution of Emergency Medical Services (EMS) has been a remarkable journey, from its humble origins to the sophisticated, highly regulated system we have today. Along this path, standardization and regulation have played a pivotal role in shaping the professional landscape of EMS.
In the early days of EMS, emergency care was fragmented and inconsistent. Patients often received care from poorly trained personnel using rudimentary equipment, and response times were unpredictable. The lack of standardized protocols and training resulted in variable patient outcomes and hindered the overall effectiveness of emergency care.
The 1960s marked a turning point with the groundbreaking work of Dr. Peter Safar on cardiopulmonary resuscitation (CPR) techniques. This revolutionary approach to patient care was a catalyst for change, prompting the National Academy of Sciences to publish a White Paper on Accidental Death and Disability.
This report highlighted the urgent need for a comprehensive EMS system, leading to the establishment of paramedic training programs in the 1970s. These programs provided advanced medical training to pre-hospital personnel, enhancing their ability to deliver life-saving interventions.
The 1970s also saw the creation of the National Registry of EMTs (NREMT), a pivotal step towards standardizing training and ensuring the competence of emergency medical technicians (EMTs). This move helped to establish a benchmark for EMS education and laid the foundation for the professionalization of the field.
In 1973, the implementation of the 911 emergency telephone number streamlined access to medical care, making it easier for people to summon help in times of crisis. This standardized approach to emergency response further improved the efficiency and effectiveness of EMS systems.
The passage of the Emergency Medical Services Systems Act in 1974 demonstrated the federal government’s commitment to developing a nationwide EMS system. This act provided funding and support for standardized protocols, training, and coordination among emergency responders, fostering a more cohesive and effective approach to patient care.
The 1980s witnessed the widespread adoption of advanced medical equipment and technology, including defibrillators and advanced airway management devices. These advancements further enhanced the capabilities of EMS providers, enabling them to deliver a higher level of care in the pre-hospital setting.
In the 1990s and beyond, the focus shifted towards evidence-based practices, quality improvement initiatives, and ongoing education for EMS providers. This commitment to continuous learning and improvement has driven the field forward, ensuring that patients receive the most up-to-date and effective care.
The rise of specialized EMS teams, such as hazardous materials response units and tactical medical teams, further demonstrates the growing professionalism and adaptability of the field. These specialized teams are equipped to handle complex emergencies and provide specialized care in challenging environments.
Today, EMS stands as a highly regulated and standardized profession, with a clear hierarchy of training and certification standards. This evolution has been driven by the dedication of EMS professionals, healthcare organizations, and government agencies working together to ensure that patients receive the highest quality of care, regardless of their location or circumstances.
Key Takeaways:
- Early EMS care was fragmented and inconsistent, leading to variable patient outcomes.
- Standardization and regulation began with Dr. Peter Safar’s work on CPR techniques and the National Academy of Sciences’ White Paper on Accidental Death and Disability.
- Paramedic training programs, the NREMT, and the implementation of 911 standardized EMS education, training, and response times.
- The Emergency Medical Services Systems Act provided federal support for standardized protocols, training, and coordination among emergency responders.
- Advanced medical equipment and technology, evidence-based practices, and specialized EMS teams have further enhanced the capabilities of EMS providers.
- Ongoing commitment to professionalization, standardization, and regulation ensures that patients receive the highest quality of EMS care.
Sources:
- Updated framework on quality and safety in emergency medicine
- National Emergency Medical Services Education Standards
Technological Advancements: The Impact of Innovations on Patient Care
In the ever-evolving realm of healthcare, technological advancements are revolutionizing the way we deliver patient care. Innovations like telemedicine, electronic health records (EHRs), and wearable health devices are redefining accessibility, convenience, and personalized care.
Telemedicine: Transforming Healthcare Delivery
Telemedicine has emerged as a powerful tool, connecting patients with healthcare professionals remotely. Virtual consultations, video conferencing, and remote patient monitoring systems empower individuals to receive care from the comfort of their own homes. This technology has proven particularly beneficial for those in rural or underserved areas, bridging the gap in access to quality healthcare services.
Electronic Health Records: The Power of Information Sharing
EHRs have revolutionized the way patient information is stored, shared, and utilized. These digital repositories consolidate medical history, test results, diagnoses, and treatment plans, providing a comprehensive view of a patient’s health journey. This streamlined access to information improves coordination among healthcare providers, reduces medical errors, and enhances the overall quality of care.
Wearable Health Devices: Empowering Patient Engagement
Wearable health devices have become indispensable tools for monitoring and tracking personal health metrics. These devices provide real-time data on heart rate, blood pressure, sleep patterns, and physical activity levels, empowering individuals to take an active role in managing their health. By leveraging this technology, patients can make informed decisions, adopt healthier lifestyles, and detect potential health issues early on.
Artificial Intelligence: Unlocking the Power of Data
Artificial intelligence (AI) algorithms are revolutionizing healthcare by analyzing vast amounts of medical data to identify patterns, predict disease risks, and assist in diagnosis, treatment selection, and drug discovery. These algorithms can sift through complex datasets, uncovering hidden insights and correlations that may have been missed by traditional methods. AI-driven systems are poised to transform healthcare by providing personalized treatment recommendations, automating administrative tasks, and enhancing clinical decision-making.
Remote Patient Monitoring: Proactive Care at a Distance
Remote patient monitoring systems allow healthcare providers to track vital signs, medication adherence, and overall health status from a distance. This technology empowers individuals to manage their chronic conditions effectively, reducing the need for frequent hospital visits. By monitoring patients remotely, healthcare providers can detect and address potential health issues proactively, preventing complications and improving outcomes.
Value-Based Care: Aligning Incentives for Better Care
Value-based care models emphasize patient satisfaction, outcomes, and cost-effectiveness, driving innovation towards personalized and efficient healthcare solutions. This approach encourages healthcare providers to focus on delivering high-quality care, reducing unnecessary procedures, and improving patient engagement. By aligning incentives, value-based care models promote a patient-centric approach to healthcare delivery.
Conclusion: The Future of Patient Care
Technological advancements are reshaping the landscape of healthcare, ushering in an era of patient-centered care, convenience, and personalization. From telemedicine to AI-driven diagnostics, these innovations are transforming the way we deliver and receive care. As technology continues to evolve, we can expect even more groundbreaking advancements that will revolutionize healthcare and improve the lives of patients worldwide.
Key Takeaways:
- Technological advancements are revolutionizing patient care by enhancing accessibility, convenience, and personalization.
- Telemedicine connects patients with healthcare professionals remotely, bridging the gap in access to quality healthcare services.
- EHRs provide a comprehensive view of a patient’s health journey, improving coordination among healthcare providers and reducing medical errors.
- Wearable health devices empower individuals to take an active role in managing their health by tracking personal health metrics.
- AI algorithms analyze vast amounts of medical data, providing personalized treatment recommendations and enhancing clinical decision-making.
- Remote patient monitoring systems allow healthcare providers to track vital signs and health status remotely, enabling proactive care and preventing complications.
- Value-based care models align incentives for better care by emphasizing patient satisfaction, outcomes, and cost-effectiveness.
- Technological advancements are transforming healthcare and will continue to revolutionize the way we deliver and receive care.
Sources:
- The Impact of Technological Advancements on Patient Care
- Telemedicine: Transforming Healthcare Delivery
Advancement in Training and Education: The Evolution of EMS Education and Certification
The healthcare landscape has undergone a remarkable transformation, and emergency medical services (EMS) have emerged as a cornerstone of modern healthcare delivery. Join me as we delve into the fascinating narrative of EMS education and certification, tracing its evolution from humble origins to the sophisticated system we have today.
In the Beginning
The roots of EMS can be traced back to the 1960s, when visionaries recognized the urgent need for standardized and regulated EMS care. This era marked the birth of paramedicine, with pioneering programs aimed at equipping pre-hospital personnel with advanced medical training.
National Registry of EMTs (NREMT)
A pivotal moment in EMS history occurred in 1970 with the establishment of the National Registry of EMTs (NREMT). This organization played a crucial role in creating a national certifying exam for EMS providers, ensuring a level of competence and consistency across the field.
The Rise of Paramedics
Despite the progress made, many believed that more could be done to enhance the capabilities of EMS providers. This led to the development of the paramedic role, a specialized position with advanced skills training, including the ability to administer medications and perform invasive procedures.
Growing Demand for Training
As interest in EMS soared, an increasing number of individuals sought training in CPR, EMT, and paramedic programs. This surge in demand highlighted the importance of ensuring quality standards in EMS education, leading to the accreditation of paramedic programs.
Challenges and Changes
The evolution of EMS education was not without its challenges. Some programs faced accreditation issues or closures due to various factors. Additionally, the EMT-P curriculum underwent periodic updates, including revisions in 1985, 1988, and 2000, to reflect evolving practices and advancements in the field.
Key Takeaways:
- The establishment of the National Registry of EMTs (NREMT) in 1970 marked a significant step towards standardizing EMS care.
- The introduction of paramedic programs provided advanced medical training to pre-hospital personnel, enhancing their capabilities.
- Accreditation of paramedic programs ensured adherence to quality standards, fostering confidence in the education provided.
- Ongoing curriculum updates, such as those in 1985, 1988, and 2000, reflected the dynamic nature of EMS practices.
Sources:
- Birth of EMS: The History of the Paramedic
- Paramedics in the United States
FAQ
Q1: How did the development of CPR techniques impact EMS?
A1: In 1966, Dr. Peter Safar introduced his groundbreaking work on CPR. This marked a pivotal moment as it standardized and improved resuscitation techniques, leading to better patient outcomes.
Q2: What role did the National Academy of Sciences play in the evolution of EMS?
A2: In 1967, the National Academy of Sciences released a White Paper on Accidental Death and Disability. This report highlighted the urgent need for a comprehensive EMS system, emphasizing training, standardized protocols, and coordination among emergency responders.
Q3: How did the passage of the Emergency Medical Services Systems Act impact EMS development?
A3: In 1974, the United States Congress passed the Emergency Medical Services Systems Act. This act provided federal funding and support for the development of EMS systems nationwide, leading to significant improvements in pre-hospital care.
Q4: What was the significance of establishing the National Registry of EMTs (NREMT)?
A4: The creation of the National Registry of EMTs in the 1970s was a milestone in EMS history. It established a national certification process for EMTs, ensuring standardized training and competence among emergency medical personnel.
Q5: How did the implementation of the 911 emergency telephone number impact EMS?
A5: In 1973, the first 911 emergency telephone number was introduced in the United States. This centralized system for reporting emergencies greatly improved response times and access to emergency care.