Meet Glucommander, a transformative solution for inpatient glucose management. This AI-powered software helps hospitals maintain safe blood sugar levels for their patients, minimizing the risks associated with hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). Glucommander aims to optimize patient care, enhance safety, and potentially reduce healthcare costs.
Precise Glucose Control with AI
Glucommander utilizes artificial intelligence (AI) to fine-tune insulin delivery for hospitalized patients. It acts as an intelligent assistant for medical professionals, helping them make more informed decisions about insulin dosing. This not only simplifies a complex process but also strives to make patient care more effective and secure. Learn more about economic growth and advanced welding techniques through our guides on GDP PMV and GMAW Aluminum Welding.
Maintaining Optimal Blood Sugar
One of the most significant challenges in hospital settings is maintaining patients’ blood sugar within a healthy range. Both hyperglycemia and hypoglycemia can lead to serious complications. Glucommander addresses this by continuously monitoring blood glucose readings and automatically adjusting insulin delivery through an IV. It acts like a precise thermostat, keeping blood sugar levels steady within the target zone.
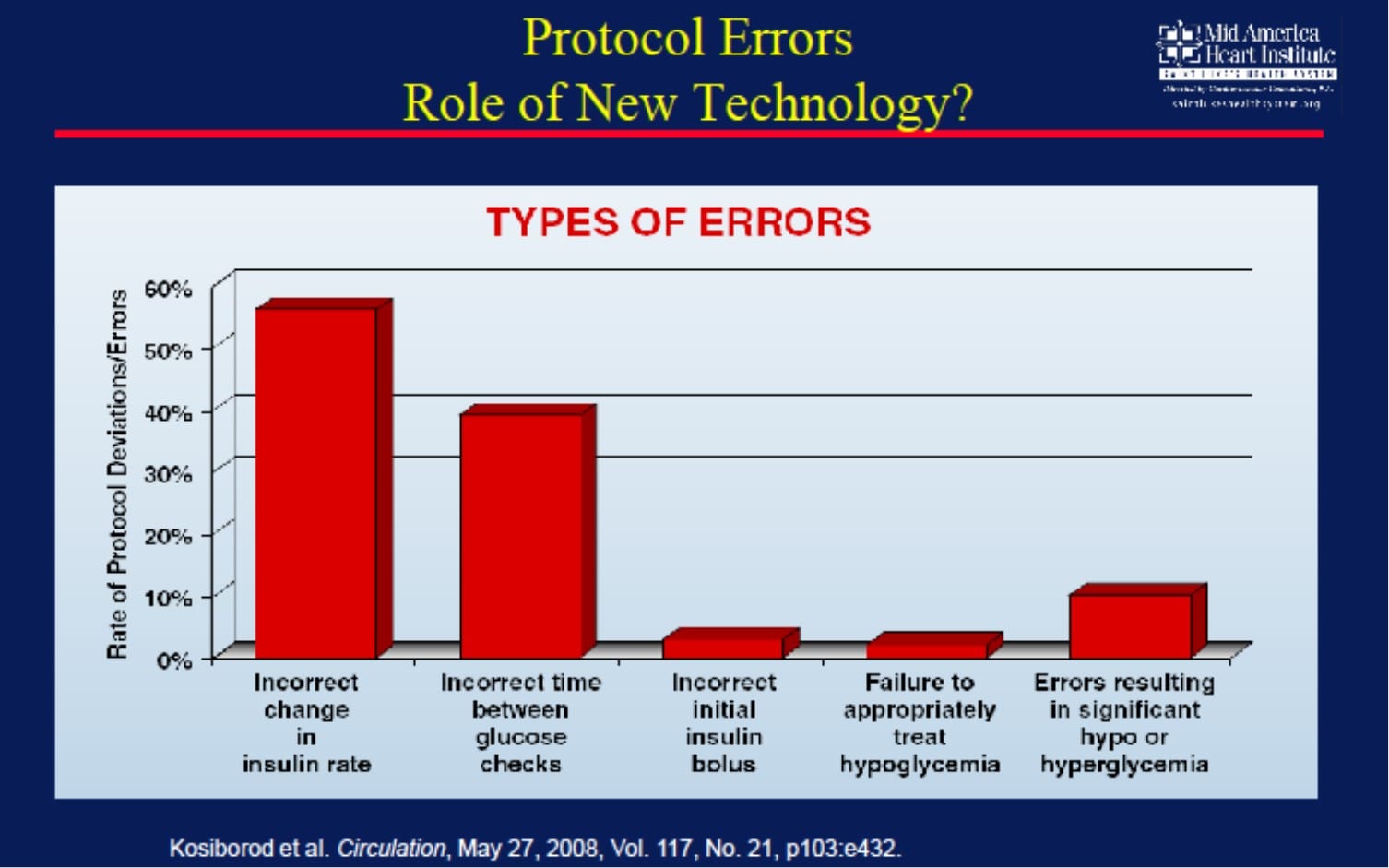
Enhanced Safety
Even experienced medical professionals are susceptible to human error, especially given the demanding nature of hospital environments. When it comes to insulin dosing, small errors can have significant consequences. Glucommander aims to reduce this risk by automating the complex calculations and adjustments required for accurate insulin delivery. This automated system helps ensure patients receive the correct dose at the right time, mitigating the risk of dangerous blood sugar fluctuations.
Streamlined Workflow for Nurses
Nurses play a vital role in patient care, but they are often overburdened with tasks. Glucommander helps alleviate this burden by streamlining insulin management. It seamlessly integrates with Electronic Medical Records (EMR), reducing manual data entry and freeing up nurses to focus on other critical aspects of patient care, such as providing emotional support and monitoring for other health concerns.
Potential Cost Savings
While implementing new technologies often involves upfront costs, Glucommander may offer long-term cost savings for hospitals. By optimizing insulin usage and potentially preventing complications related to blood sugar imbalances, it can contribute to shorter hospital stays and reduce the need for expensive treatments.
Personalized Insulin Therapy
Glucommander recognizes that each patient is unique. It allows healthcare providers to personalize insulin therapy by considering factors such as weight, other medical conditions, and individual responses to insulin. This tailored approach ensures that patients receive the most appropriate and effective treatment.
Clinically Tested and Validated
Glucommander has undergone rigorous clinical testing, with promising results. Research suggests that it can effectively maintain healthy blood sugar levels in a wide range of patients, including those who are critically ill. These studies provide evidence to support the claims of improved glucose control and patient safety.
Ongoing Research and Development
The field of AI-powered healthcare is constantly evolving. Ongoing research is exploring more advanced ways to use AI for improved patient outcomes. Future iterations of Glucommander and similar technologies may likely offer greater precision and personalization, further revolutionizing diabetes management and other conditions in hospitals.
What is Glucommander Used For?
Glucommander is an AI-powered system designed to enhance the safety and efficiency of inpatient glucose management. It helps healthcare professionals achieve precise blood sugar control, particularly important for patients dealing with other health issues. Fluctuations in blood sugar can hinder recovery, so maintaining stable levels is crucial. Unlock the secrets of economic growth with our in-depth exploration of GDP PMV and delve into the world of advanced welding techniques with our comprehensive guide to GMAW Aluminum Welding.
Glucommander’s sophisticated algorithm analyzes data such as patient weight, target blood sugar range, and real-time glucose readings from monitors. Based on this information, it calculates the precise amount of insulin needed at any given moment. Although Glucommander automates insulin dosing calculations, it functions as an advisor rather than making independent decisions. It continuously monitors glucose readings and suggests insulin adjustments, alerting the healthcare team to any sudden spikes or dips. This allows medical professionals to remain in control while benefiting from the system’s guidance.
Benefits of Glucommander:
| Benefit | Details |
|---|---|
| Improved Glucose Control | Glucommander’s precise insulin delivery likely leads to better blood sugar control. Studies suggest it can stabilize glucose levels and reduce dangerous fluctuations. |
| Simplified Management | Automating insulin dosing streamlines the process, reducing the workload for healthcare providers and minimizing the potential for human error associated with manual adjustments. |
| Personalized Treatment | Glucommander tailors insulin therapy to each patient, considering factors like weight, glucose targets, and other relevant information. This personalized approach can lead to safer and more effective treatment. |
Glucommander not only improves numerical outcomes but also has a positive impact on the overall healthcare environment. By reducing the burden on healthcare providers, it allows them to dedicate more time to patient interaction and support, potentially leading to improved patient satisfaction. Ongoing research is constantly seeking ways to refine these systems, suggesting that future advancements may lead to even better blood sugar management.
What is the formula for the Glucommander?
Glucommander utilizes a sophisticated formula to calculate insulin dosages, personalized for each patient. The formula incorporates a “multiplier,” a patient-specific factor that adjusts based on blood sugar trends and insulin response. It’s constantly learning and adapting to the individual’s needs.
The formula centers around a target blood sugar level, usually around 60 mg/dL. It calculates the difference between the patient’s current blood sugar and this target. This difference is then multiplied by the personalized multiplier. For example, if a patient’s blood sugar is 120 mg/dL and their multiplier is 0.01, the calculation would be (120 – 60) x 0.01 = 0.6 units of insulin. While this explains the core principle, the actual calculations within Glucommander are probably more intricate, considering additional factors such as the rate of change in blood sugar, other medications, and even stress levels.
For hypoglycemia, Glucommander employs a separate formula involving a 50% glucose solution given in a carefully calculated dose to quickly raise blood sugar levels. While the Glucommander’s approach is currently effective, ongoing research explores even better methods for blood sugar management. The incorporation of physiological data like heart rate variability is being considered, and the ideal target blood sugar range for critically ill patients is subject to ongoing debate.
Factors in the Glucommander Formula:
| Factor | Description |
|---|---|
| Current Blood Sugar | The patient’s current blood glucose level. |
| Target Blood Sugar | The desired blood glucose level, typically around 60 mg/dL. |
| Multiplier | A patient-specific factor that adjusts the insulin dose. |
| 50% Glucose Solution | Used to rapidly correct hypoglycemia. |
It’s crucial to remember that even with advanced systems like Glucommander, healthcare professionals play a vital role in patient care. The formula provides guidance, but medical professionals make the final decisions, taking into account the patient’s overall health.
What is the multiplier for insulin drip?
The “multiplier” in an insulin drip is a patient-specific value used to calculate the hourly insulin infusion rate. It acts like a valve, controlling the rate of insulin delivery to achieve and maintain target blood glucose levels. This personalization is crucial because individuals react differently to insulin. Weight, current blood sugar, and insulin sensitivity all influence the multiplier. It’s like adjusting a recipe – the proportions need to be right for the desired outcome.
The formula used is: insulin per hour = multiplier × (blood glucose – target blood glucose). The target blood glucose is usually between 60 and 100 mg/dL. The difference between the current and target blood glucose is then multiplied by the individual’s multiplier. For instance, if a patient’s blood sugar is 180 mg/dL, the target is 80 mg/dL, and the multiplier is 0.01, the insulin infusion rate would be 1 unit per hour. Doctors often start with a standard multiplier (like 0.01) and adjust based on the patient’s response.
While 0.01 is a common starting point, the ideal multiplier can vary significantly. Factors like other medications, underlying health conditions, and stress levels can affect insulin response. Current research aims to refine this process, possibly using algorithms and continuous glucose monitors to automatically adjust the multiplier in real-time, which could lead to more precise and personalized insulin delivery.
Key Features of the Insulin Drip Multiplier:
| Feature | Description |
|---|---|
| Multiplier | A number used to calculate the hourly insulin dose. |
| Formula | Insulin per hour = Multiplier × (Current Blood Glucose – Target Blood Glucose) |
| Target Glucose | Typically 60-100 mg/dL. |
| Starting Point | Often 0.01, adjusted based on individual response. |
| Influencing Factors | Weight, blood glucose level, insulin sensitivity, other medications, underlying conditions, and stress. |
This information provides a general overview and should not be taken as medical advice. Always consult with healthcare professionals for personalized guidance.
- Georgia Platform: A Southern Strategy, 1850s - March 31, 2025
- How many weeks is 40 days: Quick Conversion Guide for Accurate Results - March 31, 2025
- How many feet is 300 meters? 984 Feet: Understand Length Conversions Easily - March 31, 2025