This guide provides comprehensive instruction on finger thoracostomy, a life-saving procedure used in emergency situations to address tension pneumothorax and hemothorax. We’ll cover everything from the steps involved to the pros, cons, and when it’s most appropriate, aiming to give you a thorough understanding of this critical intervention.
Understanding Finger Thoracostomy
Finger thoracostomy is a life-saving emergency procedure performed to relieve pressure on a collapsed lung. This pressure can be caused by a tension pneumothorax (air buildup) or a hemothorax (blood in the chest cavity). This procedure is often a critical bridge to more definitive treatment, such as chest tube insertion.
How Finger Thoracostomy Works
Preparation: The medical professional ensures a sterile environment, using gloves, gown, and drapes. Local anesthetic and a scalpel are prepared. Patient consent is obtained if possible; in dire emergencies, implied consent is assumed.
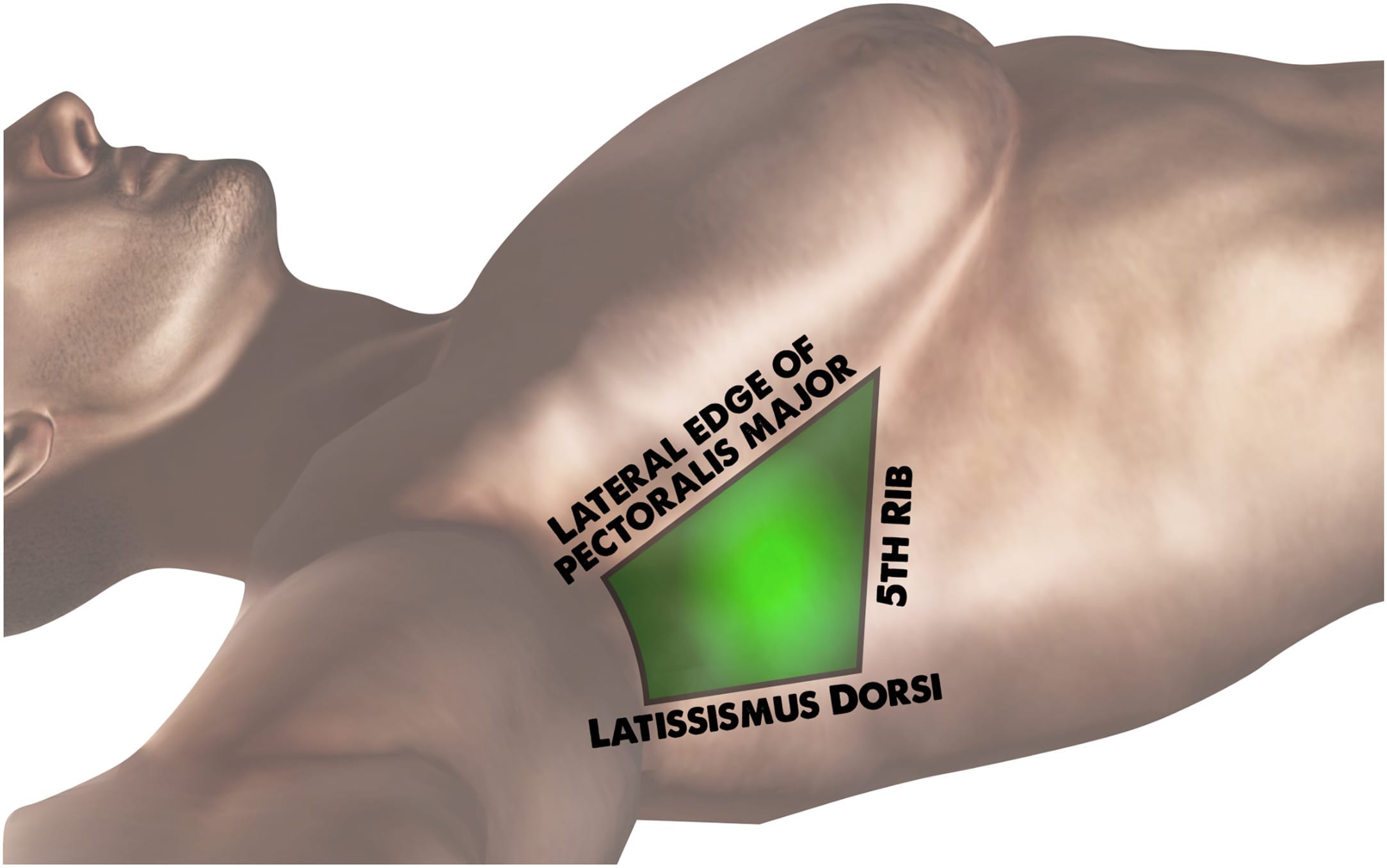
Incision: The clinician identifies the correct intercostal space (between the ribs) and makes a small incision, sometimes using a needle first.
Insertion & Decompression: A gloved finger is carefully inserted into the incision to clear the pleural space (area between lung and chest wall). The finger also helps confirm lung re-inflation and checks for abnormalities. This allows trapped air or blood to escape, relieving pressure.
Monitoring: Throughout the procedure, the patient’s vital signs are closely monitored, and supplemental oxygen is likely administered.
Weighing the Benefits and Risks
| Advantages | Disadvantages |
|---|---|
| Confirms entry into the pleural space. | Risk of infection if sterility is not maintained. |
| Creates a larger opening for drainage, particularly beneficial for hemothorax. | Possibility of bleeding. |
| Less likely to block compared to needle thoracostomy. | Risk of lung injury if the finger is not inserted correctly. |
| Can be painful. |
When is Finger Thoracostomy Necessary?
- Tension Pneumothorax: Life-threatening pressure buildup around the lung.
- Hemothorax: Blood accumulation in the chest cavity.
- Facilitating Chest Tube Insertion: May be performed prior to chest tube insertion for easier access.
When is Finger Thoracostomy Not Recommended?
- Bleeding Disorders (Coagulopathy): Increased risk of uncontrolled bleeding.
- Chest Deformities: May hinder access to the correct area.
- Cooperative Patients: Less invasive procedures like needle thoracostomy might be preferred if the patient’s condition allows and the setting is more controlled.
Paramedics and Finger Thoracostomy
Finger thoracostomy is a procedure that paramedics can perform in specific, life-threatening situations, typically involving tension pneumothorax or hemothorax. While it sounds invasive, it’s a crucial intervention executed by trained professionals who understand the anatomy and potential risks. It’s important to note that less invasive methods are preferred when the patient is stable and time permits.
When Paramedics May Perform Finger Thoracostomy:
| Situation | Likelihood of Finger Thoracostomy | Rationale |
|---|---|---|
| Tension Pneumothorax | High | Offers immediate pressure relief and life-saving potential. |
| Hemothorax | High | Aids in removing blood and improving breathing. |
| Difficulty Inserting Chest Tube | High | Can facilitate chest tube placement. |
| Bleeding Disorders | Low | Increased risk of uncontrolled bleeding. |
| Chest Deformities | Low | Procedure may be more difficult or risky. |
| Stable Patient, Other Options Available | Low | Less invasive procedures are preferred when possible. |
Steps in Paramedic-Performed Finger Thoracostomy:
Preparation: Sterilization of the area, potential use of local anesthetic, and securing patient consent (when feasible).
Incision: A small incision between the ribs.
Pleural Space Entry: Careful insertion of a gloved finger to confirm entry.
Decompression: Allowing trapped air or blood to escape, relieving pressure.
Paramedics must make rapid, informed decisions based on the specific situation. Ongoing research suggests refinements to these techniques may emerge in the future. The ability of paramedics to perform finger thoracostomy is a vital tool in prehospital emergency medicine, significantly improving patient survival odds.
Needle Decompression vs. Finger Thoracostomy
Both needle decompression (ND) and finger thoracostomy (FT) relieve pressure in the chest caused by air or fluid buildup (tension pneumothorax, hemothorax, etc.), acting as temporary solutions until a chest tube can be placed. They differ in how they access the pleural space: ND uses a needle, while FT involves a small incision and finger insertion.
Procedure Details:
Needle Decompression:
Preparation: Sterilization, local anesthetic, and patient consent (if possible).
Needle Insertion: Precise needle insertion into the pleural space using anatomical landmarks.
Decompression: Air or fluid escapes through the needle.
Finger Thoracostomy:
Incision: A small incision between the ribs.
Finger Entry: Gentle finger insertion to widen the opening and confirm pleural space entry.
Decompression: Air or fluid escapes through the larger opening.
Comparing the Pros and Cons
| Technique | Pros | Cons |
|---|---|---|
| Needle Decompression | Quick, less invasive, minimal equipment required. | Less effective in certain situations, risk of inaccurate placement, doesn’t always confirm pleural access. |
| Finger Thoracostomy | Direct confirmation of pleural entry, larger opening for drainage. | More invasive than ND, requires anatomical knowledge. |
Ongoing research continues to refine these techniques. Some studies suggest FT may be more effective in some cases, while others emphasize ND’s speed. The choice depends on the patient, resources, and provider expertise.
Needle Thoracostomy vs. Thoracostomy (Chest Tube)
Both needle thoracostomy and thoracostomy (chest tube insertion) address the buildup of air or fluid in the pleural space, but they differ in approach. Needle thoracostomy is a quick, temporary fix, while thoracostomy is a more permanent solution.
Needle thoracostomy uses a large needle to release trapped air or fluid, offering rapid decompression. Thoracostomy, or chest tube insertion, involves a small incision and tube placement for continuous drainage.
Key Differences
| Feature | Needle Thoracostomy | Thoracostomy (Chest Tube) |
|---|---|---|
| Invasiveness | Less invasive | More invasive |
| Speed | Faster | Slower |
| Drainage | Immediate, temporary | Continuous, long-term |
| Setting | Often prehospital | Typically hospital |
| Anesthesia | Local (may be used) | Usually general |
| Purpose | Temporary relief | Definitive treatment |
Procedure Steps
Needle Thoracostomy:
- Preparation: Cleaning and antiseptic application, possible local anesthetic.
- Needle Insertion: Insertion into pleural space.
- Aspiration: Air/fluid escapes.
- Removal and Dressing: Bandage application.
Thoracostomy:
- Preparation & Anesthesia: Cleaning, prepping, usually general anesthesia.
- Incision: Small incision between ribs.
- Tube Insertion: Chest tube placed into pleural space.
- Drainage System Connection: Tube connected to drainage system.
- Securing & Dressing: Tube secured and dressed.
Pros and Cons
Needle Thoracostomy:
- Pros: Quick, easy, less invasive.
- Cons: Temporary, may not suffice for severe cases.
Thoracostomy:
- Pros: Effective for larger volumes, continuous drainage.
- Cons: More invasive, requires general anesthesia, longer recovery.
The best choice depends on the individual situation, severity, patient health, and available resources. Ongoing research continues to refine these procedures.
hepatic surgery requires a skilled surgeon experienced with the hepatorenal recess. For more information on fmx dental, visit our website.
- Senior at What Age: Benefits & Eligibility Guide - March 29, 2025
- Unlocking Senior Benefits: How Old is a Senior? Your Complete Guide - March 29, 2025
- Master Russian Politeness:A Guide to Saying Please - March 29, 2025












1 thought on “Finger Thoracostomy: A Life-Saving Emergency Procedure for Tension Pneumothorax”
Comments are closed.