This guide explores everything you need to know about chondr/o, the combining form relating to cartilage—the resilient connective tissue vital for joint health and smooth movement. From understanding its structure and function to exploring related medical conditions and treatments, this comprehensive resource provides valuable insights into maintaining optimal cartilage health. [https://www.lolaapp.com/cimbasso] [https://www.lolaapp.com/beer-lahai-roi]
What is Chondr/o?
chondr/o, derived from the Greek word khondros, simply means “cartilage.” This seemingly small term unlocks a wealth of understanding about our skeletal system, joint function, and a range of medical conditions. Grasping its meaning is essential for navigating medical terminology related to cartilage disorders and treatments. Cartilage, denoted by chondr/o, acts as a biological shock absorber, minimizing friction between bones.
Types of Cartilage and Their Roles
Cartilage isn’t uniform; there are three main types, each designed for specific functions:
- Hyaline Cartilage: The most common type, hyaline cartilage provides the smooth, gliding surface in most joints (knees, elbows) and structural support in the nose and ribs.
- Elastic Cartilage: True to its name, this flexible cartilage gives shape and support to the ears and epiglottis (the flap preventing food from entering the trachea).
- Fibrocartilage: The strongest type, fibrocartilage withstands pressure and acts as a shock absorber in intervertebral discs and menisci (knee).
Specialized cells called chondrocytes are responsible for producing and maintaining the cartilage matrix, ensuring its smooth operation and resilience.
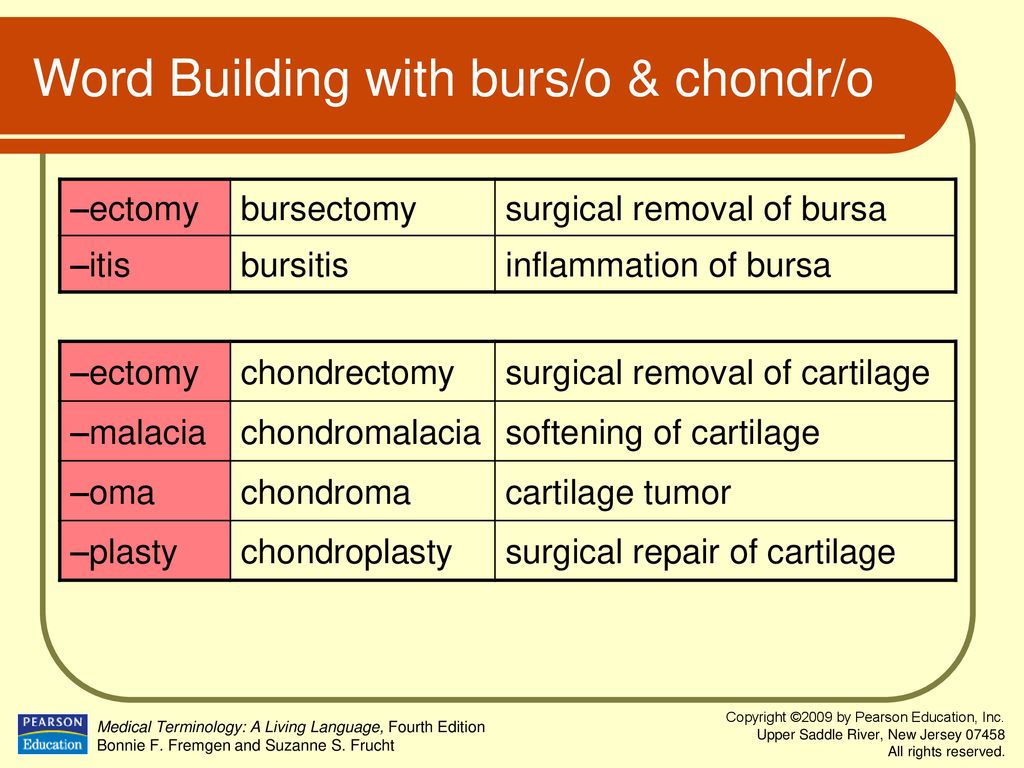
Decoding Medical Terms with Chondr/o
Understanding chondr/o helps decipher medical jargon related to cartilage health. Here are key examples:
- Chondrosis: This term signifies cartilage degeneration. Doctors utilize the Outerbridge Classification (Grades I-IV based on MRI findings) to assess the severity of cartilage damage, from minor surface irregularities to exposed bone. Risk factors for chondrosis may include obesity and repetitive strain. Treatment options range from managing pain and inflammation with medication to physical therapy for improved joint function, and potentially surgical intervention.
- Chondromalacia: Specifically referring to cartilage softening, chondromalacia commonly affects the patella (kneecap), often causing pain and discomfort.
- Chondroblast: These are immature cartilage cells that develop into chondrocytes and are crucial for producing new cartilage tissue.
- Chondrotomy: This denotes a surgical incision made into cartilage, either for diagnostic purposes or as part of a larger surgical repair.
Conditions Impacting Cartilage
Several conditions can compromise cartilage health, leading to joint issues:
- Osteoarthritis: Often referred to as “wear and tear” arthritis, osteoarthritis involves the progressive breakdown of cartilage over time.
- Rheumatoid Arthritis: An autoimmune disease where the body’s immune system attacks its own joints, damaging cartilage and surrounding tissues.
- Traumatic Injuries: Direct impacts or twisting injuries can cause acute cartilage damage.
Diagnosing Cartilage Damage
Several methods aid in diagnosing cartilage damage:
- MRI (Magnetic Resonance Imaging): Provides detailed images of cartilage and surrounding structures.
- X-ray: Can reveal joint space narrowing and bone spurs, indirect indicators of cartilage damage.
- Arthroscopy: A minimally invasive surgical procedure allowing direct visualization of joint structures and cartilage.
Protecting Your Cartilage: Tips and Strategies
Safeguarding your cartilage is a long-term investment in joint health. Consider these preventative measures:
- Weight Management: Maintaining a healthy weight reduces stress on joints, lessening the risk of cartilage damage.
- Regular Exercise: Low-impact activities like swimming and cycling strengthen supporting muscles without excessive joint stress.
- Balanced Nutrition: A diet rich in fruits, vegetables, and lean protein provides essential nutrients for cartilage health. Some research suggests vitamin D and omega-3 fatty acids may be beneficial, though further investigation is needed.
The Future of Cartilage Repair
Ongoing research explores promising avenues for cartilage regeneration, including stem cell therapy and tissue engineering. While aging naturally leads to some cartilage deterioration, proactive lifestyle choices can minimize its impact and maintain healthy joints.
This information provides a general overview and should not substitute professional medical advice. Always consult a healthcare professional for diagnosis and treatment of any cartilage-related concerns.
- Unlocking Francis Alexander Shields’ Finance Empire: A Comprehensive Biography - July 12, 2025
- Unveiling Francis Alexander Shields: A Business Legacy - July 12, 2025
- Francis Alexander Shields’ Business Career: A Comprehensive Overview - July 12, 2025