The ventral thecal sac, the protective sheath surrounding your spinal cord’s front, houses cerebrospinal fluid vital for nourishment and cushioning. Compression of this sac, extending from the foramen magnum to the second sacral vertebra, can disrupt this flow and impinge on nerve roots, potentially leading to serious neurological issues. This comprehensive guide will explore the causes, symptoms, diagnosis, and treatment of ventral thecal sac compression, empowering you with the knowledge to seek appropriate care.
What is the Ventral Thecal Sac?
The ventral thecal sac is the anterior (front) part of the thecal sac, a durable membrane encompassing the spinal cord, cauda equina (a bundle of nerves at the spinal cord’s base), and cerebrospinal fluid (CSF). This sac, formed by the dura mater (outer layer) and arachnoid mater (inner layer), acts like a protective cushion. The CSF within provides buoyancy, acts as a shock absorber, delivers nutrients, and removes waste products, ensuring the spinal cord’s health. Discover if you can truly conquer a tooth infection with the surprising properties of Listerine and learn will Listerine kill tooth infection.
Why is Ventral Thecal Sac Compression a Concern?
Ventral thecal sac indentation, often caused by disc herniation, spinal stenosis, or tumors, disrupts this vital system. It can restrict CSF flow and put pressure on delicate nerve roots. This disruption can lead to various neurological problems, ranging from pain and numbness to more serious complications.
What Causes Ventral Thecal Sac Compression?
Several conditions can lead to compression or indentation of the ventral thecal sac. Some of the most common include:
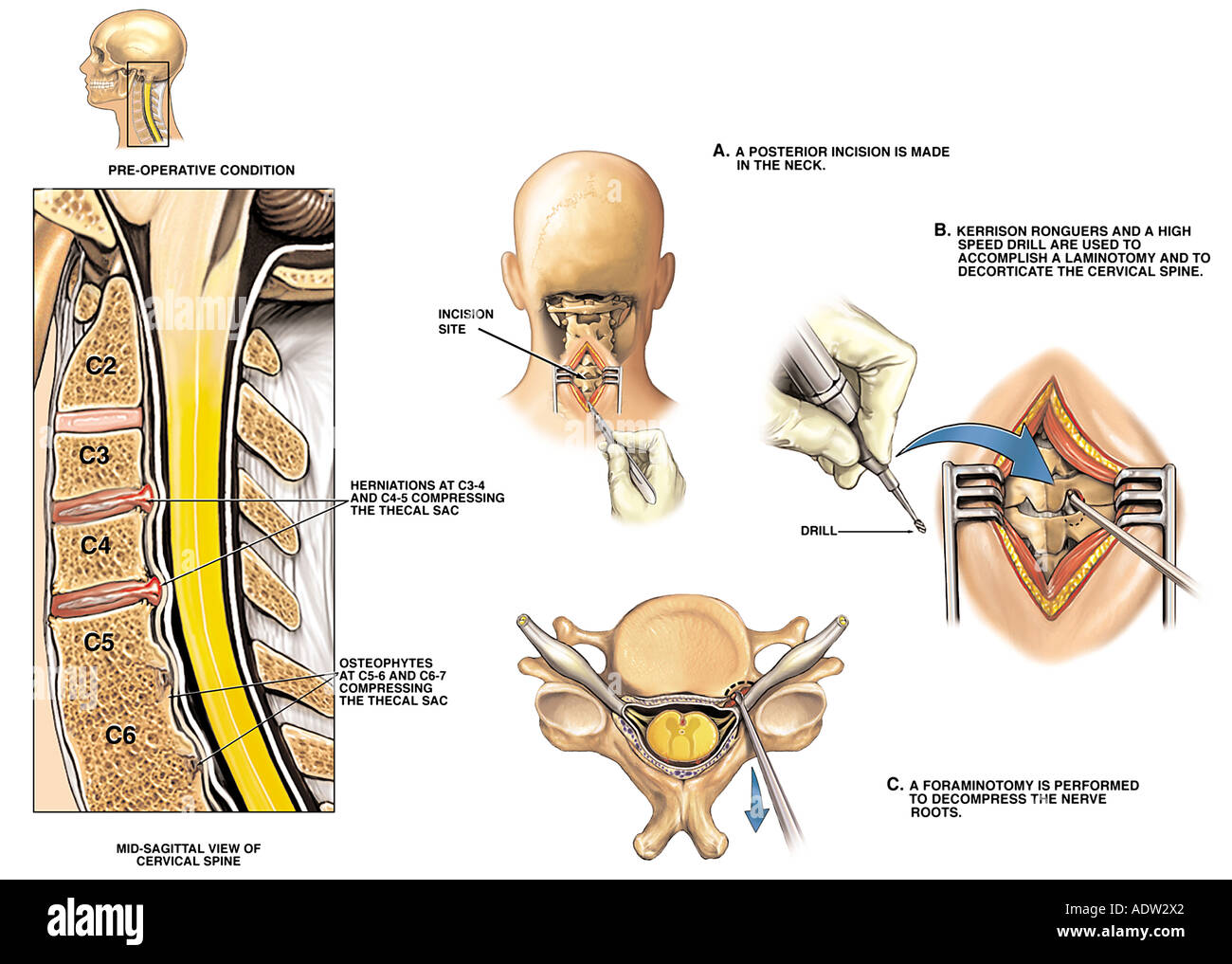
- Disc Herniation: A ruptured or bulging disc, often described as a “slipped disc,” can press against the thecal sac.
- Spinal Stenosis: Narrowing of the spinal canal, often due to age-related changes, can compress the thecal sac.
- Spinal Tumors: While less common, tumors within the spinal canal can impinge on the sac.
- Spondylolisthesis: This occurs when one vertebra slips forward over another, potentially causing compression.
- Trauma: Injuries such as car accidents or falls can cause swelling and bleeding that constricts the space around the spinal cord.
- Osteophytes (Bone Spurs): Bony outgrowths on the vertebrae, often associated with arthritis, can narrow the spinal canal and compress the thecal sac.
- Ligamentum Flavum Hypertrophy: Thickening of this ligament, which runs along the back of the spinal canal, may contribute to stenosis and compression.
Recognizing the Symptoms
Symptoms of ventral thecal sac compression vary depending on the location and severity of the compression. Some people experience mild discomfort, while others have debilitating pain. Common symptoms include:
- Pain: This can range from localized back pain to radiating pain that shoots down the legs (sciatica) or arms. The pain may be sharp, burning, or aching.
- Numbness and Tingling: These sensations can occur in the buttocks, legs, feet, groin, or arms and hands.
- Muscle Weakness: You might experience difficulty walking, lifting objects, or performing other tasks requiring strength.
- Bowel/Bladder Dysfunction: In severe cases, particularly with cauda equina syndrome (compression of the nerves at the end of the spinal cord), you might have difficulty controlling your bladder or bowels. This is a medical emergency requiring immediate attention.
Symptoms based on Location:
- Cervical Spine (Neck): Neck pain, arm pain, numbness or tingling in hands and fingers, weakness in arms or hands.
- Thoracic Spine (Mid-Back): Mid-back pain, pain radiating around the chest or rib cage, numbness or tingling in the torso.
- Lumbar Spine (Lower Back): Lower back pain, sciatica, numbness or tingling in feet and toes, weakness in legs or feet, bowel or bladder problems (in severe cases).
Diagnosing Ventral Thecal Sac Compression
Accurate diagnosis of ventral thecal sac compression requires a combination of physical examination and advanced imaging techniques. Your doctor will likely:
- Discuss your medical history and symptoms.
- Perform a physical exam to assess your reflexes, muscle strength, and range of motion.
- Order imaging studies such as:
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues, including the spinal cord, nerves, and discs, making it the preferred method for diagnosing ventral thecal sac compression.
- CT (Computed Tomography) Scan: Better at visualizing bone, making it helpful in cases involving bony spurs or fractures. A CT myelogram, where contrast dye is injected into the spinal canal, can also provide detailed images.
- X-rays: Although less detailed than MRI or CT, X-rays can rule out fractures or other bone abnormalities.
Exploring Treatment Options
Treatment for ventral thecal sac compression aims to relieve pressure on the nerves and restore normal function. The best approach depends on the underlying cause and severity of the compression.
Conservative Treatments:
Conservative treatments are often the first line of defense, particularly for mild to moderate cases. These may include:
- Pain Management: Over-the-counter pain relievers (like ibuprofen or naproxen) or prescription medications can help manage discomfort.
- Physical Therapy: Targeted exercises and stretches can strengthen supporting muscles, improve flexibility, and alleviate pressure on the thecal sac.
- Epidural Steroid Injections: These injections deliver medication directly to the affected area, helping to reduce inflammation and pain around the compressed nerves.
- Activity Modification: Avoiding activities that aggravate symptoms can help prevent further compression and promote healing.
Surgical Treatments:
If conservative treatments fail to provide sufficient relief or if the compression is severe, surgery may be necessary. Minimally invasive techniques are often preferred. Some common surgical procedures include:
- Discectomy: Removal of the herniated portion of a disc pressing on the thecal sac.
- Laminectomy: Removal of a small portion of the lamina (bone forming the back of the spinal canal) to create more space for the spinal cord and nerves.
- Spinal Fusion: Joining two or more vertebrae together to stabilize the spine, often performed in cases of instability or spondylolisthesis.
- Foraminotomy: Widening the openings (foramina) where nerve roots exit the spinal canal, relieving pressure on the nerves.
| Treatment | Description | Potential Benefits | Potential Risks |
|---|---|---|---|
| Pain Management | Medications to reduce pain signals. | Provides temporary pain relief. | May have side effects depending on the specific medication. |
| Physical Therapy | Exercises and stretches to improve strength, flexibility, and range of motion. | Strengthens muscles, improves mobility, and may reduce pain long-term. | May be time-consuming and require consistent effort. |
| Injections | Targeted injections of medication, such as steroids, to reduce inflammation and pain. | Can provide significant, although often temporary, pain relief. | May have side effects, and relief may not be long-lasting. |
| Discectomy | Surgical removal of a portion of a herniated disc. | Relieves pressure on the spinal cord and nerves. | Infection, bleeding, nerve damage, recurrence of herniation. |
| Laminectomy | Surgical removal of a portion of the lamina to widen the spinal canal. | Relieves pressure on the spinal cord and nerves. | Infection, bleeding, nerve damage, spinal instability. |
| Spinal Fusion | Surgical joining of two or more vertebrae. | Stabilizes the spine and reduces pain caused by instability. | Infection, bleeding, nerve damage, non-union of the fusion. |
The Future of Ventral Thecal Sac Compression Treatment
Ongoing research continually refines our understanding of spinal conditions like ventral thecal sac compression and their treatments. Scientists are exploring new surgical techniques, minimally invasive procedures, and regenerative therapies to improve outcomes and reduce recovery times. While there is much we know, there is also much to learn, and future discoveries hold promise for even more effective and personalized treatments.
Conclusion
Ventral thecal sac compression can be a debilitating condition, but with proper diagnosis and treatment, many individuals find significant relief and can return to their normal activities. If you are experiencing symptoms suggestive of ventral thecal sac compression, it is essential to consult a qualified healthcare professional for a thorough evaluation and personalized treatment plan. They can accurately assess your condition, discuss the potential benefits and risks of different treatment options, and guide you toward the best course of action for your individual needs. Remember, knowledge is power, and understanding your condition is the first step toward effective management.