Pregnancy is a joyous journey, but it’s also a time of potential complications. One such complication that can arise during labor is tachysystole, a condition involving excessively frequent uterine contractions. Understanding this condition is crucial for both expectant parents and healthcare professionals. This article provides comprehensive information about tachysystole, including its causes, effects, management, and ongoing research.
What is Tachysystole?
Defining Tachysystole
Tachysystole is clinically defined as six or more uterine contractions within a 10-minute period, sustained over at least 30 minutes. This differs from a brief flurry of contractions; it’s a persistent pattern of rapid uterine activity. It’s important to note that previous terms like “hyperstimulation” and “hypercontractility” lacked precision, and the standardized definition of tachysystole has greatly improved research and clinical management. This consistent, rapid squeezing of the uterus is what can potentially pose a risk to the baby. The 30-minute timeframe helps ensure there’s enough time between contractions for the uterus to relax and allow proper blood flow to the baby.
Why Does Tachysystole Occur?
Several factors can contribute to tachysystole. One of the most common is the administration of labor-inducing or augmenting medications, such as oxytocin (Pitocin) and misoprostol (Cytotec). While these medications are vital for assisting labor progression, they can sometimes overstimulate the uterus. Even epidurals, despite their pain-relieving purpose, can occasionally increase contraction frequency. Surprisingly, tachysystole can also arise spontaneously, even without medication, in naturally occurring labors. Current research is exploring potential underlying causes and risk factors, including genetic predisposition and specific maternal health conditions, to improve prediction and prevention.
Effects and Management of Tachysystole
How Tachysystole Affects Your Baby
During each contraction, the uterus temporarily tightens, briefly reducing blood flow to the placenta, the baby’s lifeline for oxygen and nutrients. Frequent, intense contractions, characteristic of tachysystole, prolong this restriction of blood flow. This can lead to fetal hypoxia (low oxygen levels) and acidosis (increased blood acidity), potentially causing immediate and long-term health problems for the baby. Ongoing research is investigating the full scope of the long-term developmental consequences of fetal hypoxia and acidosis.
Managing Tachysystole
Prompt management of tachysystole is essential. If medications are the cause, the first step is typically to reduce or discontinue them. Tocolytics, medications that relax the uterine muscles, are sometimes administered to slow down contractions, giving the baby a chance to recover. Continuous fetal monitoring plays a crucial role, allowing the medical team to closely track the baby’s heart rate and well-being throughout the process.
Diagnosing and Addressing Concerns
Recognizing Tachysystole
Healthcare professionals diagnose tachysystole using continuous monitoring of both uterine contractions and the baby’s heart rate. This allows for prompt detection and intervention. External tocodynamometry or internal intrauterine pressure catheters (IUPC) are used to measure uterine activity, correlating it with fetal heart rate patterns observed via electronic fetal monitoring. Check out our article on assessing and managing PQRST pain which can help you understand pain assessment during labor.
Addressing Concerns and Providing Support
Experiencing tachysystole can be understandably stressful for expectant mothers. Open communication with healthcare providers is vital. Don’t hesitate to ask questions and express any concerns. Emotional support during this time is just as important as medical management.
What is the Meaning of Tachysystole?
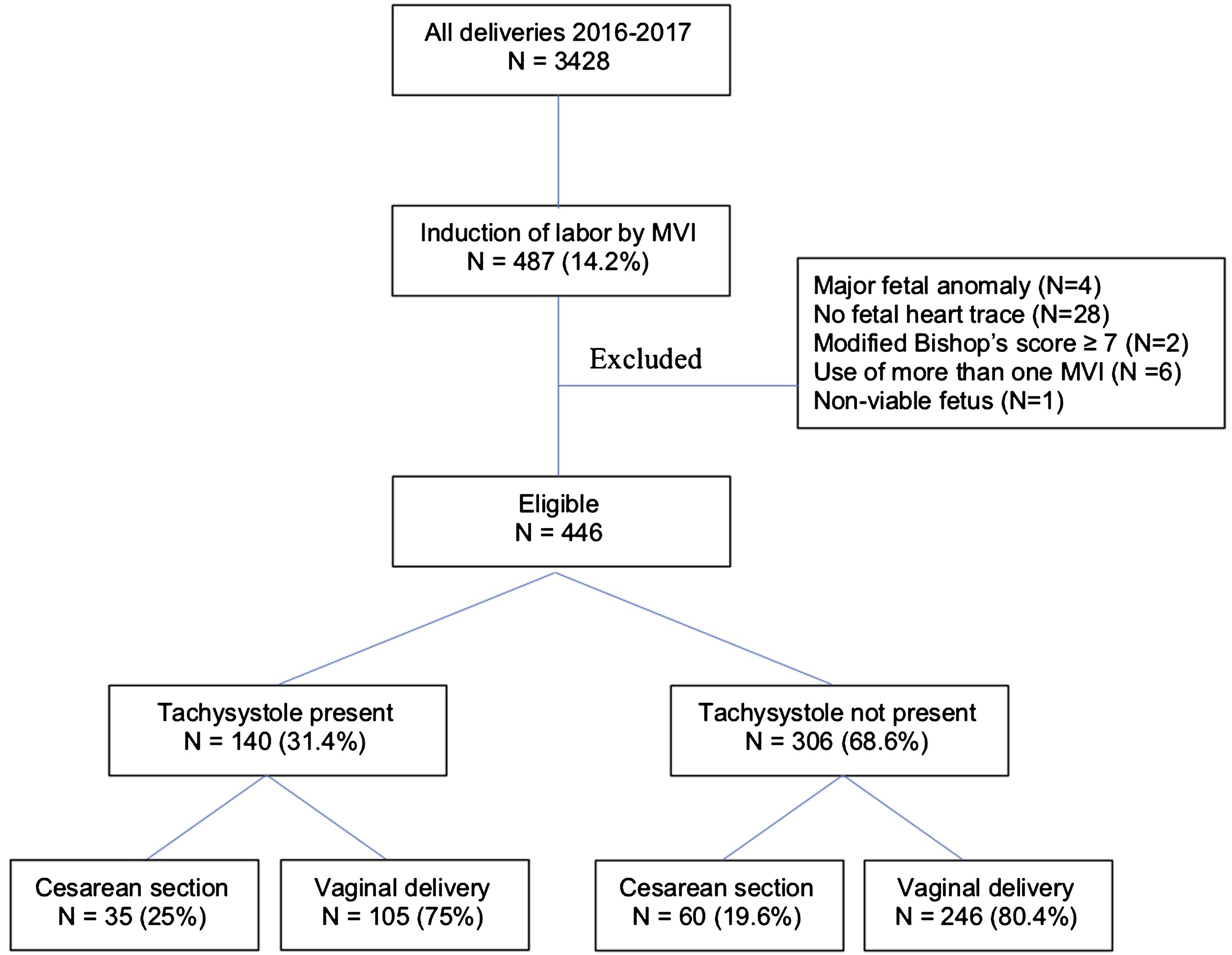
Tachysystole simply means “too many contractions.” Specifically, it refers to more than five uterine contractions in 10 minutes, averaged over a 30-minute window. This standardized definition, affirmed by the American Congress of Obstetricians and Gynecologists (ACOG) in 2009, replaced less precise terms like “hyperstimulation” and “hypercontractility,” improving research and treatment. A study found a clear link between tachysystole (defined as six or more contractions in 10 minutes within the first four hours of induction) and adverse infant outcomes. While often associated with medically induced or augmented labor, it’s crucial to remember that tachysystole can occur spontaneously, highlighting the need for diligent monitoring throughout labor.
What is the Difference Between Tachysystole and Hyperstimulation?
While the terms are related, they aren’t interchangeable. Tachysystole refers specifically to the frequency of contractions, while hyperstimulation focuses on the effect of these contractions (often combined with hypertonus – increased tension between contractions) on the baby, specifically a nonreassuring fetal heart rate. Tachysystole can lead to hyperstimulation if it significantly compromises fetal well-being, but it doesn’t always. Both conditions can be triggered by labor-inducing medications like oxytocin, but other factors such as infection or placental problems might also play a role. Effective management of both tachysystole and hyperstimulation is crucial, with interventions ranging from adjusting medication to administering tocolytics.
| Feature | Tachysystole | Hyperstimulation |
|---|---|---|
| Definition | >5 contractions in 10 minutes (averaged over 30 minutes) | Nonreassuring fetal heart rate pattern due to excessive uterine activity (often including tachysystole and hypertonus) |
| Impact | May lead to fetal distress if severe | Indicates fetal distress |
| Management | Monitoring, potential intervention | Immediate intervention to reduce uterine activity and improve fetal oxygenation |
Further research is exploring the nuances of nonreassuring fetal heart rate patterns and expanding the understanding of causes beyond oxytocin use.
[!NOTE]
This information is for general knowledge and does not replace professional medical advice. Consult your doctor or midwife for any concerns about your pregnancy or labor. Have you ever wondered what woolly bear caterpillars turn into? These fuzzy creatures undergo a fascinating transformation.
What are the Criteria for Tachysystole?
The diagnostic criteria for tachysystole are precise: six or more contractions in a 10-minute period, averaged over 30 minutes. This consistent, rapid contraction pattern restricts the uterus’s ability to relax between contractions, compromising blood flow to the placenta and potentially leading to fetal oxygen deprivation. While oxytocin administration is a common cause, tachysystole can occur spontaneously, especially as labor progresses. One study found that 43% of women undergoing induction experienced at least one 10-minute period with six or more contractions in the first four hours. Accurate diagnosis involves continuous monitoring of both fetal heart rate and uterine contractions. Management strategies range from adjusting oxytocin dosages to administering tocolytic medications. Research continues to explore the long-term effects of tachysystole on newborns and refine management protocols.












1 thought on “Uterine Tachysystole: Understanding, Managing, and Minimizing Risks During Labor”
Comments are closed.