Procalcitonin (PCT) is a powerful tool in modern medicine, used to identify and manage bacterial infections, especially the life-threatening condition known as sepsis. It acts as a crucial guide for antibiotic therapy, ultimately improving patient outcomes. Unlike traditional inflammatory markers, PCT offers high sensitivity and specificity for bacterial infections, enabling earlier and more targeted interventions. By understanding how PCT works, healthcare professionals can leverage this biomarker to optimize antibiotic stewardship, reduce unnecessary antibiotic use, and combat antimicrobial resistance.
Understanding Procalcitonin: The Body’s Alarm System
PCT is a prohormone of calcitonin, typically produced at low levels by the C-cells of the thyroid gland. Its levels rise significantly in response to systemic inflammation triggered primarily by bacterial infections, playing a minimal role in viral infections or non-infectious inflammatory conditions. This characteristic makes it an invaluable tool for differentiating between bacterial and viral infections, a distinction that can often be challenging but is crucial for determining the appropriate course of treatment. If you want to learn more about the ways the radprimer can be applied to your research, be sure to check it out!
How PCT Works
During bacterial infections, immune cells like macrophages and monocytes release PCT into the bloodstream. The exact mechanism isn’t fully understood, but bacterial toxins and inflammatory mediators likely stimulate this release. PCT levels rise rapidly within hours of infection onset, typically peaking around 24-48 hours, and then decline with effective treatment. This rapid response makes PCT a valuable tool for monitoring treatment efficacy and adjusting antibiotic regimens as needed. While PCT is the precursor to calcitonin, their functions are distinct. Calcitonin regulates calcium levels, while PCT serves as a critical inflammatory marker.
PCT’s Role in Diagnosis and Management
PCT has revolutionized the approach to bacterial infections and sepsis. From diagnosis to discharge, PCT serves as a dynamic biomarker, guiding antibiotic duration and monitoring treatment response in bacterial infections. It’s not a magic bullet, but it provides invaluable insights for quicker, more informed decisions, leading to better patient outcomes.
Diagnosing Infections
PCT aids in the early detection of bacterial infections, especially sepsis. It helps distinguish between bacterial and viral infections, reducing the unnecessary prescription of antibiotics—a significant factor in the fight against antibiotic resistance. This is particularly crucial in sepsis diagnosis where rapid intervention is paramount. This distinction not only helps individual patients but also contributes to the broader effort to preserve the effectiveness of antibiotics for future generations.
Managing Infections
PCT isn’t just for diagnosis; it also plays a crucial role in managing infections. Doctors use PCT levels as a roadmap, guiding them in deciding when to start and, perhaps more importantly, when to stop antibiotics. PCT-guided antibiotic stewardship reduces unnecessary antibiotic use, minimizing antibiotic resistance development and improving patient outcomes. This targeted approach helps ensure that antibiotics are used only when necessary and for the appropriate duration, further contributing to the fight against antibiotic resistance. If you are interested in learning more about how to get the mchat scoring, click the link!
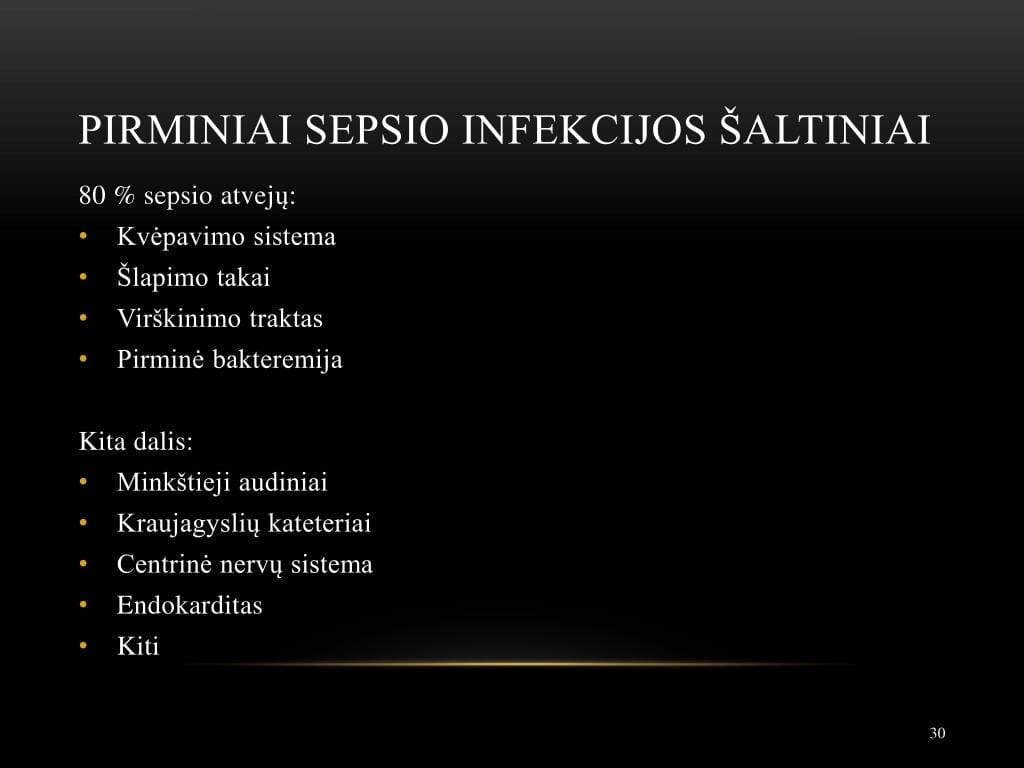
PCT and Sepsis: A Lifesaving Connection
Sepsis is a life-threatening condition arising from a dysregulated immune response to infection. Early detection is paramount, and PCT acts as a highly sensitive indicator for serious infections that may lead to sepsis. Dynamic PCT monitoring, not just single measurements, reveals critical insights into sepsis progression and patient prognosis, enabling earlier and more targeted interventions.
Beyond a Single Value: Tracking PCT Trends
Repeated PCT measurements throughout a hospital stay are crucial for capturing the dynamic trends of sepsis. These trends offer more profound insights than a single measurement, much like tracking the temperature of a pot on a stove over time tells you more than a single temperature reading. Decreasing PCT levels typically suggest a positive response to treatment, while stable or increasing levels may indicate the need for treatment adjustments or further investigation.
PCT’s Impact on Sepsis Care
PCT empowers clinicians to differentiate sepsis from systemic inflammatory response syndrome (SIRS), ensuring accurate diagnosis and timely treatment initiation. PCT-guided antibiotic stewardship is key to combatting antibiotic resistance and minimizing adverse events in sepsis, promoting better patient outcomes and cost-effectiveness. This guidance helps reduce unnecessary antibiotic use, minimizing the development of antibiotic resistance and improving overall patient safety. Research suggests that PCT guidance can lead to a reduction in antibiotic treatment duration for sepsis and lower respiratory tract infections (LRTIs), particularly for patients in intensive care units (ICUs), which also helps in antibiotic stewardship.
PCT Testing and Interpretation
PCT testing is a simple blood test analyzed in a laboratory. Elevated levels suggest bacterial infection, but the specific thresholds for interpretation depend on the clinical context. Serial measurements are usually more informative than single readings for tracking disease progression and treatment response. While highly valuable, PCT isn’t a standalone diagnostic tool. Doctors consider the patient’s symptoms, medical history, and other test results, using PCT as one piece of the diagnostic puzzle.
Advantages and Limitations of PCT
PCT offers several advantages: high sensitivity and specificity for bacterial infections, rapid response to infection status changes, and guidance for antibiotic stewardship. However, it’s essential to recognize its limitations. PCT levels can be elevated in some non-infectious conditions like severe trauma, pancreatitis, fungal infections, and certain cancers. Therefore, careful clinical interpretation in conjunction with other diagnostic tests and the patient’s clinical presentation is crucial. There is debate about the optimal PCT cutoff values for various conditions, and ongoing research is further refining our understanding of PCT and its clinical applications.
Ongoing Research and Future Directions
Ongoing research constantly refines our understanding of PCT and explores its potential in diverse areas. Some experts believe PCT may help predict the severity of infections, allowing for even earlier intervention. Other areas of active research include personalized medicine approaches tailoring antibiotic therapy based on individual PCT levels and other biomarkers. This research may eventually lead to even more refined and effective strategies for combatting bacterial infections and improving patient outcomes.
Key Points
- Bacterial Infection Indicator: PCT rises in response to serious bacterial infections.
- Distinguishing Infections: PCT helps differentiate between bacterial and viral infections, reducing unnecessary antibiotic use.
- Sepsis Severity Prediction: Elevated PCT levels can predict sepsis severity, enabling early, potentially life-saving interventions.
- Diagnosis and Management: PCT is useful in diagnosing and managing other serious infections like pneumonia, meningitis, and urinary tract infections.
- Rapid Testing: PCT testing is a simple blood test with rapid results.
- Contextual Interpretation: PCT interpretation should always consider the patient’s overall clinical picture, including symptoms, medical history, and other test results.
- Not a Perfect Marker: PCT may be elevated in certain non-bacterial conditions, highlighting the need for careful interpretation.
- Ongoing Research: Continuous research refines the understanding and application of PCT in clinical practice.
This information is intended for educational purposes only and should not be considered medical advice. Always consult with a healthcare professional for any health concerns or before making any decisions related to your health or treatment.
- Crypto Quotes’ Red Flags: Avoid Costly Mistakes - June 30, 2025
- Unlock Inspirational Crypto Quotes: Future Predictions - June 30, 2025
- Famous Bitcoin Quotes: A Deep Dive into Crypto’s History - June 30, 2025














1 thought on “Procalcitonin (PCT): A Key Biomarker for Bacterial Infections and Sepsis Management”
Comments are closed.