Decoding MR. SOPA: Essential Steps for Newborn Ventilation
When a newborn arrives, a healthy cry signals robust lungs. But sometimes, babies need help taking their first breath. Neonatal resuscitation, guided by the Neonatal Resuscitation Program (NRP), provides that critical support, with MR SOPA as a core element. Think of MR SOPA as a structured checklist for healthcare providers, ensuring newborns receive the oxygen they need. This guide explains MR SOPA and its importance in optimizing neonatal ventilation. For those interested in other aspects of performance improvement, resources like the Navy Eval Manual can offer valuable insights.
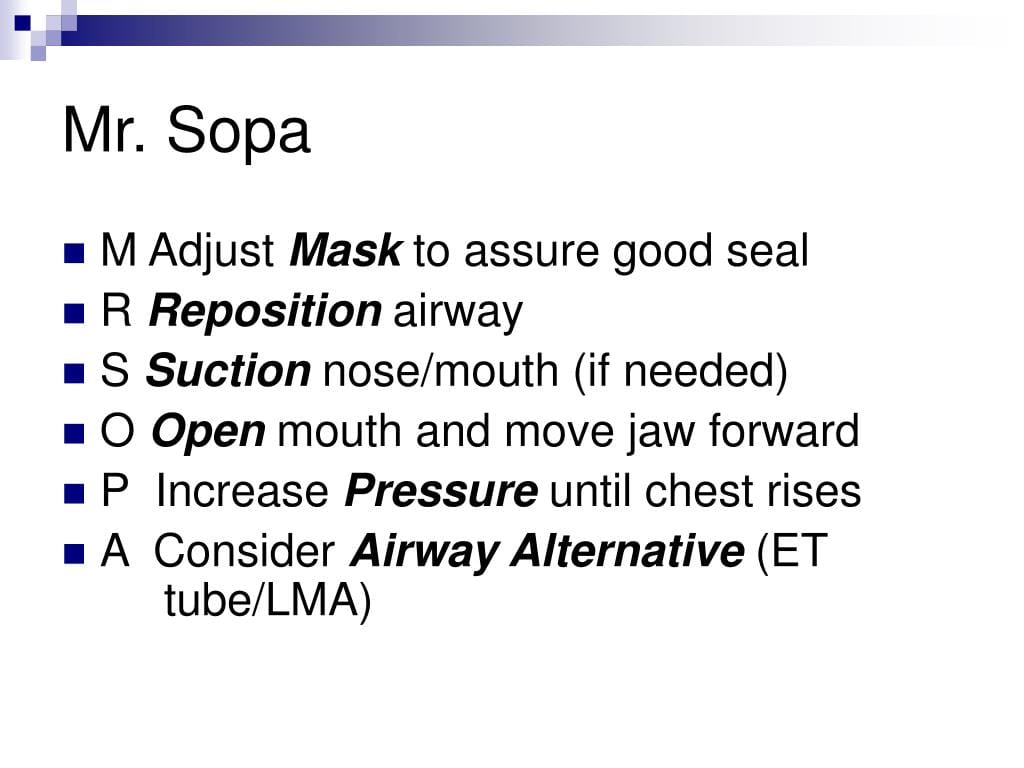
What is MR SOPA in NRP?
Positive pressure ventilation (PPV) helps newborns inflate their lungs. However, PPV isn’t always immediately effective. MR SOPA is a mnemonic, a memory aid, guiding healthcare providers through corrective steps when PPV isn’t optimal. It’s like troubleshooting a leaky balloon – finding and fixing the problem efficiently. Each letter represents a crucial action:
- M – Mask Adjustment: Ensures a proper mask seal over the baby’s nose and mouth, minimizing air leaks. This often involves a two-handed technique.
- R – Reposition Airway: Positions the baby’s head in the “sniffing position,” aligning the airway for optimal airflow. A shoulder roll might be necessary for some infants.
- S – Suction Mouth and Nose: Clears secretions from the mouth and nose using a bulb syringe, removing potential obstructions to breathing.
- O – Open Mouth: Gently opens the baby’s mouth, maintaining airway patency and ensuring airflow isn’t restricted.
- P – Pressure Increase: Carefully increases the ventilation pressure in increments, typically 5-10 cm H2O, up to a maximum of 40 cm H2O (Peak Inspiratory Pressure or PIP), aiming for a visible chest rise with each breath.
- A – Alternative Airway: If mask ventilation remains ineffective, an alternative airway, such as an endotracheal tube (ETT) or laryngeal mask airway (LMA), might be necessary. This is typically performed by experienced medical personnel.
MR SOPA is crucial because it provides a systematic, step-by-step approach to troubleshooting PPV challenges. This structured method helps ensure consistent and effective care, maximizing the newborn’s chances of breathing effectively. For a deeper understanding of optimizing ventilation in other contexts, exploring the differences highlighted in guides like “newsies jr script” can be enlightening.
MR SOPA in Action: A Step-by-Step Guide
- Initial PPV: Begin PPV with a properly sized mask.
- Assessment: Observe chest rise, heart rate, and oxygen saturation. If inadequate after approximately 30 seconds, initiate MR SOPA.
- MR SOPA Steps: Systematically apply each step – Mask, Reposition, Suction, Open, Pressure, Alternative airway – reassessing ventilation after each action.
- Advanced Interventions: If MR SOPA is unsuccessful, more advanced interventions, including medications, may be necessary.
Troubleshooting Common MR SOPA Challenges
- Mask Seal: Difficulty maintaining a proper seal may suggest an improperly sized mask or require adjustments to the two-handed technique.
- Persistent Secretions: If suctioning doesn’t clear the airway, repositioning the baby or a different suctioning technique may be required.
- Suboptimal Chest Rise with Increased Pressure: This suggests a possible obstruction or underlying lung issue requiring further investigation and intervention.
The “Why” Behind MR SOPA: Understanding the Physiology
- Mask Adjustment: A proper seal minimizes air leaks, ensuring delivered breaths effectively reach the lungs.
- Repositioning Airway: Aligning the airway reduces resistance to airflow, making breathing easier.
- Suctioning: Removing secretions clears the path for air to enter the lungs.
- Opening the Mouth: Ensures the airway isn’t obstructed by the infant’s own anatomy.
- Pressure Increase: Higher pressure helps overcome resistance and inflate the lungs, but must be carefully controlled to avoid lung injury.
- Alternative Airway: Provides a secure airway when mask ventilation fails, ensuring oxygen delivery directly to the lungs.
The Role of Teamwork in MR SOPA
Effective neonatal resuscitation requires coordinated teamwork. Clear communication, designated roles, and shared understanding of the MR SOPA algorithm are crucial for successful implementation.
| MR SOPA Step | Description | Why It’s Important |
|---|---|---|
| Mask | Ensure a proper mask seal using a two-handed technique. | Prevents air leaks and maximizes the effectiveness of delivered breaths. |
| Reposition | Position the baby’s head in the “sniffing position,” possibly with a shoulder roll. | Aligns the airway, reducing resistance to airflow and optimizing ventilation. |
| Suction | Clear secretions from the mouth and nose using a bulb syringe. | Removes obstructions that might be hindering breathing. |
| Open | Gently open the baby’s mouth, potentially lifting the jaw forward slightly | Ensures the airway remains patent and airflow isn’t restricted. |
| Pressure | Increase ventilation pressure in 5-10 cm H2O increments, not exceeding 40 cm H2O. | Helps inflate the lungs and improve oxygen delivery, but must be carefully controlled to avoid injury. |
| Alternative | Consider an alternative airway (ETT or LMA) if mask ventilation fails. | Provides a secure airway for oxygen delivery when mask ventilation is ineffective. |
Looking Ahead: Ongoing Research and Future Directions
Neonatal resuscitation is a dynamic field, and ongoing research continually refines best practices. While MR SOPA is currently a vital tool, future studies may suggest modifications or additions to the algorithm. Emerging research areas include:
- Optimized pressure settings: Studies are exploring individualized pressure strategies for different gestational ages and clinical scenarios.
- Alternative airway devices: New devices and techniques for securing the airway are constantly being developed and evaluated.
- Integration of technology: Researchers are investigating ways to incorporate technology, such as real-time feedback systems, to enhance the effectiveness of neonatal resuscitation.
This ongoing research reinforces the importance of staying current with the latest NRP guidelines and recommendations. By integrating the latest evidence-based practices, healthcare providers can continue to improve outcomes for newborns requiring resuscitation. This dedication to continuous improvement reflects the commitment to giving each newborn the best possible chance at a healthy start.
- Clovis Unified School District Calendar: A Parent’s Guide to Key Dates & Updates (2023-2026) - November 22, 2024
- Bossier Parish Schools Calendar 2024-2025: A Parent’s Guide to Key Dates & Resources - November 22, 2024
- 2024-2025 Caddo Parish School Calendar: Key Dates and Information - November 22, 2024

![[History of EMS Timeline]: A Journey from Humble Beginnings to Sophisticated Healthcare history-of-ems-timeline_2](https://www.lolaapp.com/wp-content/uploads/2023/12/history-of-ems-timeline_2-150x150.jpg)











1 thought on “Mastering MR SOPA in NRP: A Practical Guide to Optimizing Neonatal Ventilation”
Comments are closed.